|
Radiation Pneumonitis/Fibrosis
- Damage to lungs after radiation therapy
- Usually requires at least 4500 rads
- Especially common if >6000 R given in 5-6 weeks
- Occurs more often if there is concurrent or later
chemotherapy
- Pathologic phases
- Exudative phase = edema fluid + hyaline membranes
- Organizing phase
- Fibrotic phase = interstitial fibrosis
- Time of onset
- Usually at least 6 weeks up to 6 months after
treatment
- Location
- Confined to radiation portal
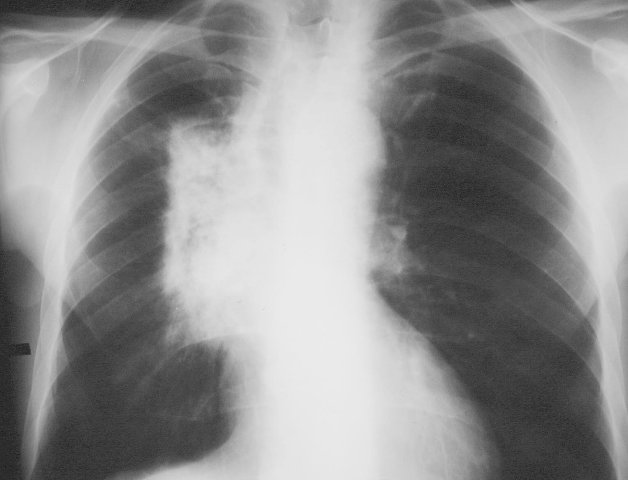 
Radiation portal (right) with subsequent radiation pneumonitis (left image).
· Acute Radiation Pneumonitis
o Occurs within 1-8 weeks after radiation therapy
o Pathology
§ Depletion of surfactant (1 week to 1 month later), plasma
exudation, desquamation of alveolar + bronchial cells
o Usually asymptomatic
o When symptomatic
§ Nonproductive cough, shortness of breath, weakness, fever
(insidious onset)
§ Acute respiratory failure (rare)
o Changes usually confined to radiation portal
o Patchy / confluent consolidation, may persist up to 1 month (exudative
reaction)
§ Atelectasis + air bronchogram
§ Spontaneous pneumothorax (rare)
- CT findings of acute radiation pneumonitis
- Homogeneous slight increase in attenuation (2-4
months after therapy)
- Patchy consolidation (1-12 months after therapy)
- Non-uniform discrete consolidation (most common; 3
months to 10 years after therapy)
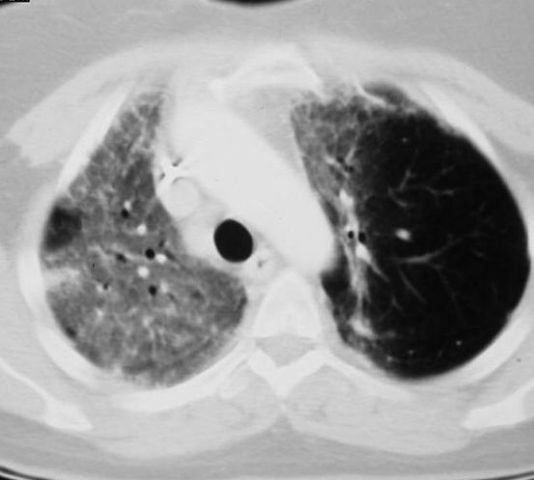 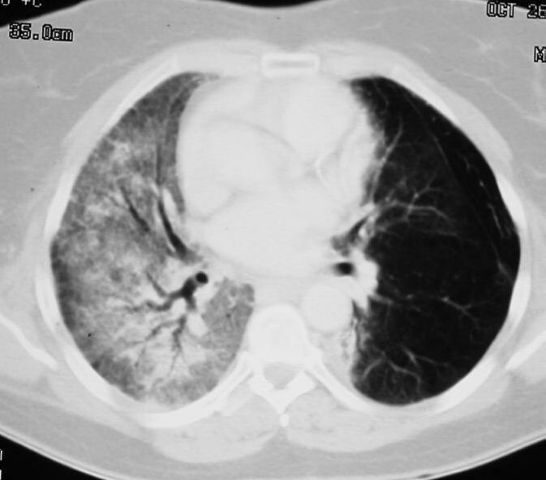 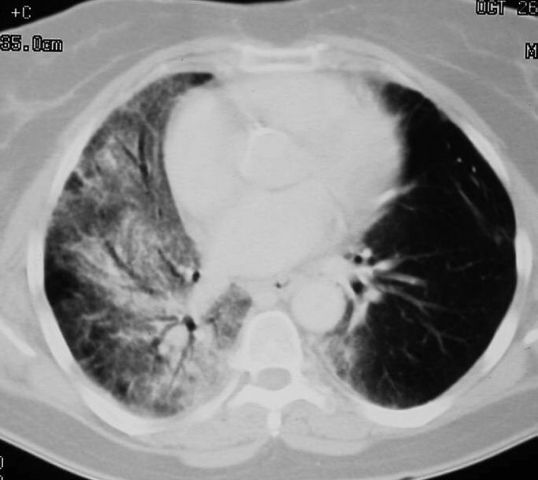
Sequential
transverse images through lung showing radiation pneumonitis in right lung
- Prognosis
- Recovery or progression to death from fibrosis
- Rx
· Chronic Radiation Damage
o 9-12 months after radiation therapy
o Histology
§ Permanent damage of endothelial + type I alveolar cells
o May be associated with:
§ Thymic cyst
§ Calcified lymph nodes (in Hodgkin disease)
§ Pericarditis + effusion (within 3 years)
§ Severe loss of volume
§ Dense fibrous strands from hilum to periphery
§ Thickening of pleura
o CT findings
§ Solid consolidation (radiation fibrosis) + bronchiectasis
(stabilized by 1 year after therapy)
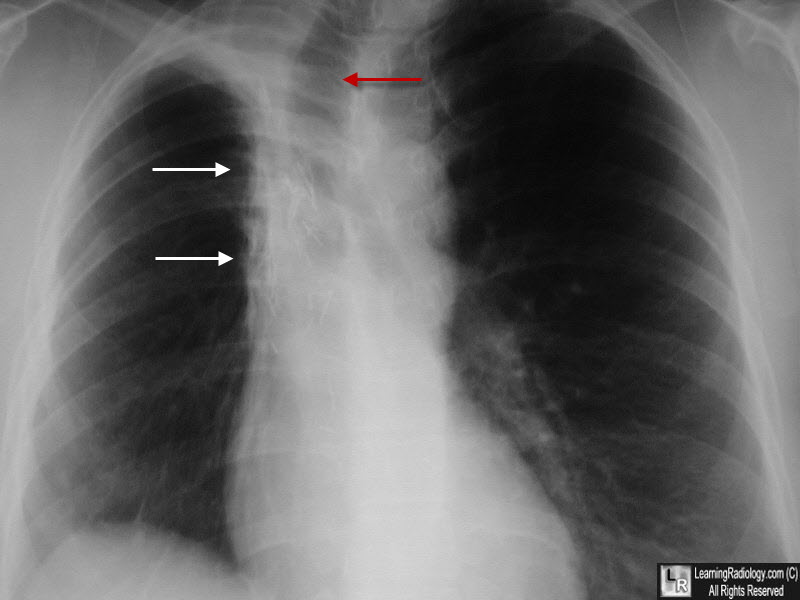
Radiation Fibrosis. There is a zone of increased density in the right paratracheal region with an almost straight edge (white arrows) suggestive of scarring from a radiation portal. The tr4achea is deviated to the right from volume loss (red arrow).
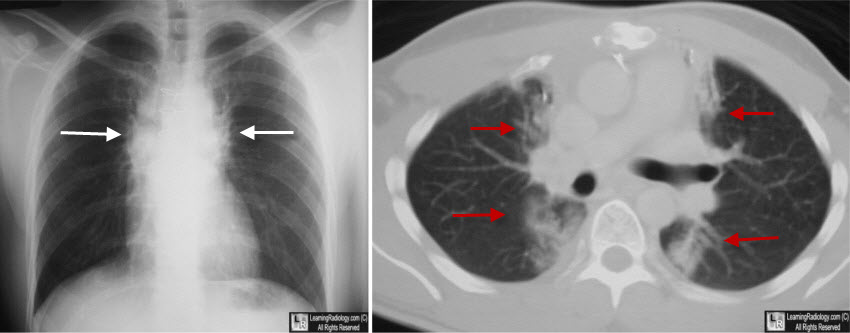
Radiation Fibrosis. The chest radiograph shows bilateral and almost symmetrical densities in a paramediastinal location with unusually well-demarcated edges, suggesting a radiation portal(white arrows). The CT scan demonstrates the same findings with fibrotic stranding seen on both sides of the mediastinum along the path of prior radiation (red arrows).
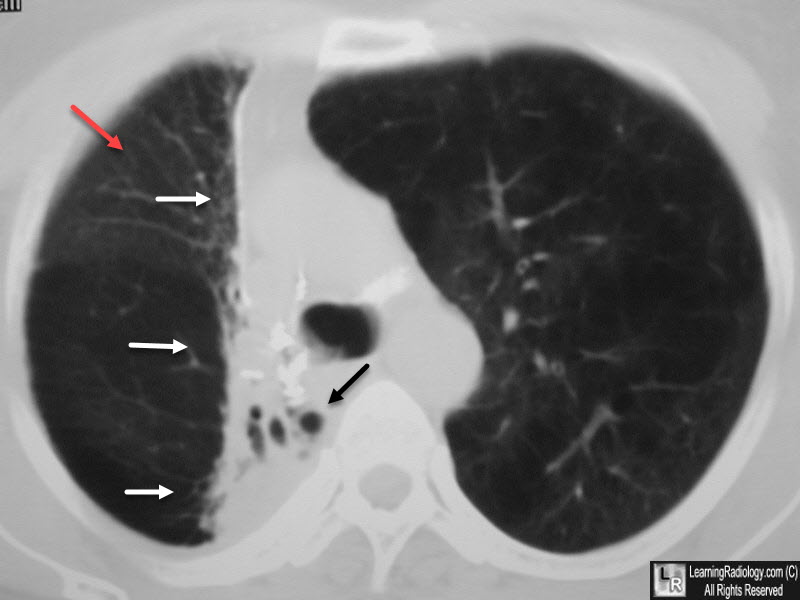
Radiation Fibrosis. The chest radiograph shows loss of volume in the right hemithorax (red arrow). There is a sharply demarcated zone of increased density along the right side of the mediastinum (white arrows) characteristic of a radiation portal. Traction bronchiectasis is present (black arrow).
|