|
|
Pneumothorax
- Presence of air in the pleural space
- Anatomy
- Visceral pleura is adherent to lung surface
- There is no air in the pleural space normally
- The introduction of air into the pleural space separates the visceral from the parietal pleura
- In contradistinction, the visceral and parietal pleura usually do not separate from each other in obstructive atelectasis
- Pathophysiology
- Either from disruption of visceral pleura
- Or, trauma to parietal pleura
- Clinical findings
- Acute onset of
- Pleuritic chest pain
- Dyspnea (in 80-90%)
- Cough
- Back or shoulder pain
- Etiologies
- Penetrating trauma
- Blunt trauma
- May be due to rib fracture
- May be caused by increased intrathoracic pressure
- May lead to bronchial rupture
- “Fallen lung sign” (ptotic lung sign) -- hilum of lung is below expected level within chest cavity
- Persistent pneumothorax with functioning chest tube
- Iatrogenic
- Tracheostomy
- Central venous catheter attempt or insertion
- Mechanical ventilation
- May occur in up to 25% of patients maintained on PEEP
- May be bilateral or under tension
- Thoracic irradiation
- Spontaneous pneumothorax
- Most common etiology
- Cause
- Rupture of subpleural blebs in apical region of lung
- Age
- 20-40 years
- M:F = 8:1
- Especially in patients who are tall and thin
- Smokers

Red arrows point to thin white visceral pleural line which
is the single best sign for a pneumothorax
- Prognosis
- Recurrence in 30% on same side
- Recurrence in 10% on contralateral side
- Treatment
- Simple aspiration (success in >50%)
- Tube thoracostomy (effective in 90%)
- Other causes of a pneumothorax
- Neonatal disease
- Meconium aspiration
- Respirator therapy for hyaline membrane disease
- Malignancy
- Primary lung cancer
- Lung metastases, especially from osteosarcoma
- Also pancreas, adrenal, Wilms tumor
- Pulmonary infections
- Tuberculosis
- Necrotizing pneumonia
- Coccidioidomycosis
- Hydatid disease
- Pertussis
- Acute bacterial pneumonia
- Staphylococcal septicemia
- AIDS (Pneumocystis carinii, Mycobacterium tuberculosis, atypical mycobacteria)
- Complication of pulmonary fibrosis
- Histiocytosis X
- Idiopathic
- Cystic fibrosis
- Sarcoidosis
- Scleroderma
- Eosinophilic granuloma
- Interstitial pneumonitis
- Rheumatoid lung
- Idiopathic pulmonary hemosiderosis
- Pulmonary alveolar proteinosis
- Biliary cirrhosis
- Asthma or emphysema
- Produce a second peak incidence of pneumothorax from 45-65 years of age
- Due to rupture of peripheral emphysematous areas
- “Catamenial pneumothorax” is a recurrent spontaneous pneumothorax that occurs during menstruation and is associated with endometriosis of the diaphragm
- Marfan’s syndrome
- Ehlers-Danlos syndrome
- Pulmonary infarction
- Lymphangiomyomatosis and tuberous sclerosis
- Incidence of pneumothorax is particularly high in lymphangiomyomatosis and histiocytosis X
- Types of pneumothorax
- Closed pneumothorax = intact thoracic cage
- Open pneumothorax = "sucking" chest wound
- Tension pneumothorax
- Accumulation of air within pleural space due to free ingress and limited egress of air
- Pathophysiology:
- Intrapleural pressure exceeds atmospheric pressure in lung during expiration (check-valve mechanism)
- Frequency
- In 3-5% of patients with spontaneous pneumothorax
- Higher in barotrauma (mechanical ventilation)

Tension pneumothorax on left (blue arrow) is displacing the heart and mediastinal structures to the right (red arrow); this case also shows a deep sulcus sign on the left (yellow arrow). There is underlying hyaline membrane disease.
- Simple pneumothorax –no shift of the heart or mediastinal structures
- Imaging findings in pneumothorax
- Must see the visceral pleural white line
- Very thin white line that differs from a skin fold by its thickness
- Absence of lung markings distal or peripheral to the visceral pleural white line
- Not evidence enough to say there is a pneumothorax only if there are no lung markings seen
- No lung markings will be seen with bullous disease
- Bullae have a concave surface facing the chest wall
- Pneumothorax almost always has a convex surface facing the chest wall
- Displacement of mediastinum and/or anterior junction line
- Deep sulcus sign
- On frontal view, larger lateral costodiaphragmatic recess than on opposite side
- Diaphragm may be inverted on side with deep sulcus
- Total / subtotal lung collapse
- This is passive or compressive atelectasis
- Collapse of SVC or IVC due to decreased systemic venous return and decreased cardiac output
- Tension hydropneumothorax
- Sharp delineation of visceral pleural by dense pleural space
- Mediastinal shift to opposite side
- Air-fluid level in pleural space on erect chest radiograph
- Radiographic signs in upright position
- White margin of visceral pleura separated from parietal pleura
- Usually seen in the apex of the lung
- Absence of vascular markings beyond visceral pleural margin
- May be accentuated by an expiratory film in which lung volume is reduced while amount of air in pneumothorax remains constant so that relative size of pneumothorax appears to increase
- Radiographic signs in supine position
- Anteromedial pneumothorax (earliest location)
- Outline of medial diaphragm under cardiac silhouette
- Deep sulcus sign
- Decubitus views of the chest may demonstrate a pneumothorax on the side that is non-dependent
- Left lateral decubitus view for right-sided pneumothorax
- Right lateral decubitus view for left-sided pneumothorax
- Subpulmonic pneumothorax (second most common location)
- Hyperlucent upper abdominal quadrant
- Deep lateral costophrenic sulcus
- Sharply outlined diaphragm in spite of parenchymal disease
- Visualization of anterior costophrenic sulcus
- Visualization of inferior surface of lung
- Apicolateral pneumothorax (least common location)
- Visualization of visceral pleural line
- Posteromedial pneumothorax (in presence of lower lobe collapse)
- Lucent triangle with vertex at hilum
- V-shaped base delineating costovertebral sulcus
- Pneumothorax outlines pulmonary ligament
- Pitfalls in diagnosis
- Skin fold
- Thicker than the thin visceral pleural white line
- Air trapped between chest wall and arm
- Will be seen as a lucency rather than a visceral pleural white line
- Edge of scapula
- Follow contour of scapula to make sure it does not project over chest
- Overlying sheets
- Usually will extend beyond the confines of the lung
- Hair braids
- Prognosis
- Resorption of pneumothorax occurs at a rate of 1.25% per day (accelerated by increasing inspired oxygen concentrations)

Tension Pneumothorax. Radiograph of the chest shows a large left-sided pneumothorax (white arrows) which is under tension as manifest as displacement of the heart to the right (black arrow) and depression of the left hemidiaphragm (yellow arrow).
For the same photo without the arrows, click here
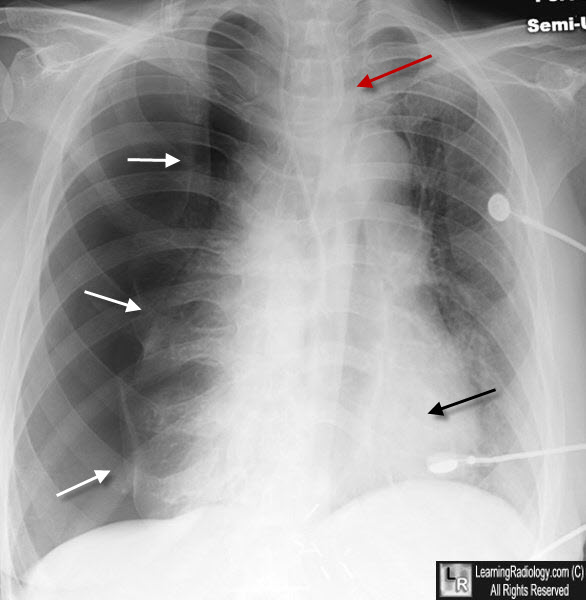
Tension Pneumothorax. Radiograph of the chest shows a large right-sided pneumothorax (white arrows) with a shift of the heart (black arrow) and trachea (red arrow) to the left.
For more information, click on the link if you see this icon 
Thoracic Radiology: The Requisites
|
|
|