|
Tuberculosis
Primary
Pulmonary Tuberculosis
§ Upper lobes affected
slightly more than lower
§
Alveolar infiltrate
§
Cavitation is rare
§ Lobar pneumonia is
almost always associated with lymphadenopathy—therefore, lobar
pneumonia associated with hilar or mediastinal adenopathy at any age should
strongly suggest TB
§ Mostly unilateral hilar
and/or paratracheal, usually right
sided, rarely bilateral
§ Differentiates primary
from postprimary TB—it does not occur in postprimary TB
§
Much more common in
children
·
Airway
· Atelectasis classically
affects the anterior segments of the upper lobes or the medial segment of the
RML
·
Pleura
§
Pleural effusion as a
manifestation of primary TB occurs more often in adults than children
§
With appropriate
treatment, it carries the best prognosis of all patterns of TB and is the
least likely to develop complications
§ The fluid accumulates
slowly and painlessly—therefore, patients
with TB are seldom seen with a small amount of pleural fluid
§
Parenchymal disease will
almost never be present with a pleural effusion although lymphadenopathy may
§ Apical pleural scarring
is rarely tuberculous in origin
Postprimary Tuberculosis (“Reactivation TB”)
Patterns
of distribution
§
Almost always affect the
apical or posterior segments of the upper lobes or the superior segments of
the lower lobes—bilateral upper lobe disease is very common
§
May present as pneumonia
§
Cavitation may result:
the cavity is usually thin-walled, smooth on the inner margin with no
air-fluid level
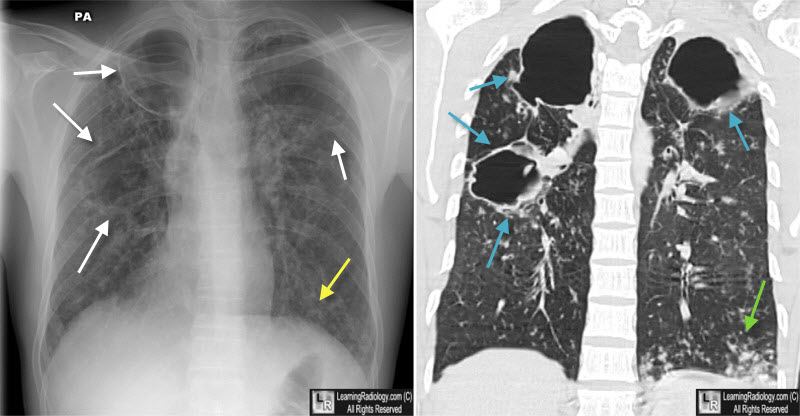
Tuberculosis, Cavitary. There are large cavities in both apices (white arrows) and airspace disease at the left base (yellow arrow) on the chest radiograph. On the coronal CT, the thin-walled upper lobe cavities without air-fluid levels are again seen (blue arrows) as is the consolidation at the left base (green arrow). Nodular densities are scattered throughout both lungs.
§
Transbronchial
spread may
occur—from one upper lobe to opposite lower or to another lobe
§
Miliary
spread (below)
§
Bronchiectasis—usually
asymptomatic
§
Bronchostenosis due to fibrosis and stricture: fibrosis may cause distortion of a bronchus and
atelectasis many years after the initial infection—“middle lobe
syndrome”
§
Solitary pulmonary
nodule—the tuberculoma—may occur
in either primary or postprimary disease; round or oval lesions with small,
discrete shadows in the immediate vicinity of the lesion—the “satellite” lesion
-
Formation
of a pleural effusion in postprimary TB almost always means direct spread
of the disease into the pleural cavity and should be regarded as an empyema—this carries a graver prognosis than the pleural
effusion of the primary form
-
Direct
extension into the ribs or sternoclavicular joints is uncommon
Miliary Tuberculosis
-
Older
men, Blacks and pregnant women are susceptible
-
Onset
is insidious
-
Fever,
chills, night sweats are common
-
Takes
weeks between the time of dissemination and the radiographic appearance of
disease
-
Considered
to be a manifestation of primary TB–although clinical appearance of
miliary TB may not occur for many years after initial infection
-
When
first visible, they measure about 1 mm in size; they can grow to 2-3mm if
left untreated
-
When
treated, clearing is rapid—miliary TB seldom, if ever, produces
calcification
TB and Other Diseases
-
There
is an association between TB and silicosis, TB and HIV
-
There
may be an association between TB and sarcoid
-
There
is no association between TB and bronchogenic carcinoma
HIV and
TB
-
No
matter what form of TB the patient has, it tends to look like 1° TB
-
Hilar
and mediastinal adenopathy are common
-
Cavitation
is less common
-
There
is no predilection for the apices
-
MAI
(mycobacterium avium-intracellulare) is more common in HIV than TB

Tuberculosis, post-primary. There are large cavities in both apices and smaller cavities scattered throughout the lungs. The lungs are over-aerated and there is already scarring present. Dilated bronchi (tuberculous bronchiectasis) is present throughout the lungs.
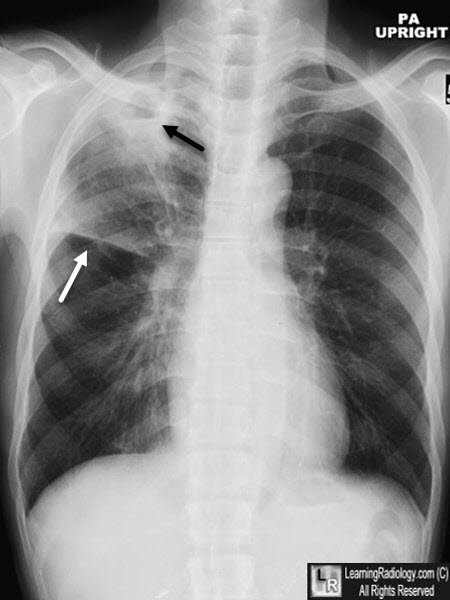
Tuberculosis, cavitary. There is a cavity in the right upper lobe with an air-fluid level (black arrow). There is volume loss in the right upper lobe as evidenced by elevation of the minor fissure (white arrow).
|