|
|
Loffler Syndrome
General Considerations
- An acute respiratory illness with peripheral blood eosinophilia, one of the causes of pulmonary infiltrates with eosinophilia (PIE)
- Originally described as a reaction to the pulmonary phase of Ascaris lumbricoides
- Also caused by drugs induced pulmonary eosinophilia
- Some of the drugs associated are
- Antimicrobials such as penicillin, tetracycline INH and nitrofurantoin
- Anticonvulsants such as Dilantin and valproic acid
- Anti-inflammatory agents such as aspirin, naproxen and ibuprofen
- Bleomycin, chlorpromazine, imipramine, sulfonamides
Other Causes of Pulmonary Infiltrates with Eosinophilia |
Idiopathic |
Acute Eosinophilic Pneumonia |
Chronic Eosinophilic Pneumonia |
Hypereosinophilic Syndrome |
Associated with Diffuse Lung Diseases |
E.g. Lupus |
Secondary to Infection |
Allergic Bronchopulmonary Aspergillosis |
Clinical Findings
- Dry cough is most common
- Fever, malaise
- Dyspnea
- Myalgia
Imaging Findings
- Unilateral or bilateral air space densities, usually peripherally located (reverse pulmonary edema)
- Transient, disappearing in 2-4 weeks
- Rarely pleural effusion, especially with nitrofurantoin toxicity
Differential Diagnosis
Prognosis
- Benign, self-limiting disease
- Symptoms usually subside in 3-4 weeks
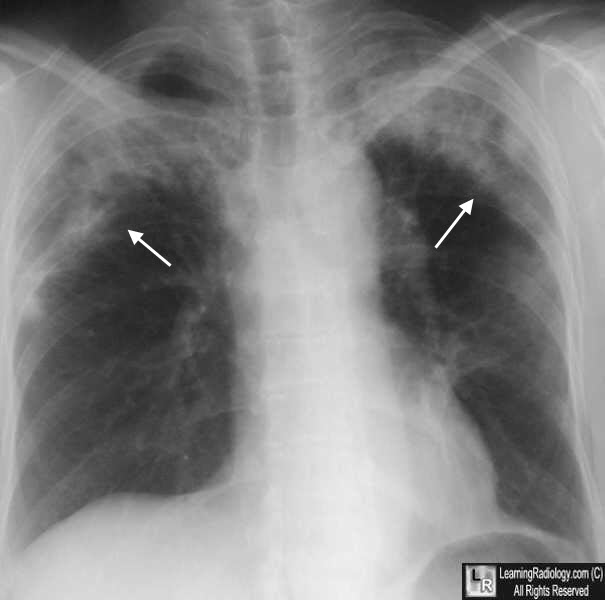
Loffler (Loeffler) Syndrome. There are bilateral peripheral infiltrates in the upper lung fields. This has been called the reverse pulmonary edema sign.
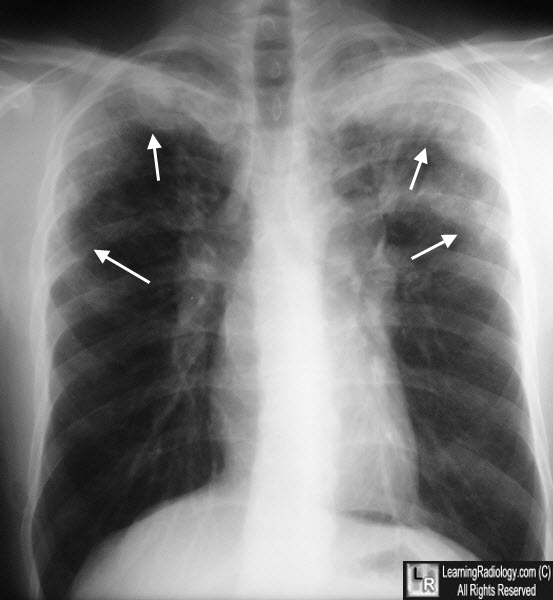
Loffler (Loeffler) Syndrome. Chest radiograph on another patient shows peripheral , primarily upper lobe airspace disease.
Eosinophilic lung diseases: a clinical, radiologic, and pathologic overview. YJ Jeong, KI Kim, IJ Seo, et al. Radiographics. 27 (3): 617-37
|
|
|