|
Lung Masses
Bronchogenic Carcinoma
- Incidence
o
On
routine survey, <5% are malignant nodules
o
At
surgery, 40% of nodules are ca, 40% granulomas
·
Causes
of lung nodules-by frequency
o
Granulomas
o
Bronchogenic
ca
o
Hamartoma
o
Metastases
·
Calcification
of lung nodules
o
Laminated:
TB granuloma
o Central
or target: histoplasmoma
o
Popcorn:
hamartoma
·
Doubling
time
o
If
a lesion doubles in volume >6 weeks and <16 months, usually malignant
·
Cavitating
nodules
o
Squamous
cell most common
o
Adenocarcinoma
o
Bronchoalveolar
cell ca (rare)
o
Hodgkin's
Disease (rare)
·
Mass
with air bronchogram
o
Alveolar
cell ca
o
Lymphoma
o
Pseudolymphoma
o
Inflammatory
pseudotumor
·
Pulmonary
nodules with pneumothorax
o
Osteosarcoma
o
Wilm's
tumor
o
Eosinophilic
granuloma
·
Types
of bronchogenic carcinoma
o
Squamous
cell ca (30-35%)
o
Adenocarcinoma
(25-35%)
o
Small
cell or oat cell (25%)
o
Large
cell undifferentiated (10%)
·
Squamous
cell ca
o
Central
Location (2/3)
o
Atelectasis
o
"Reverse
S sign of Golden"
o
Post-obstructive
pneumonia
o
Mass
o
Peripheral
location (1/3)
o
May
cavitate
o
Most
closely associated with smoking
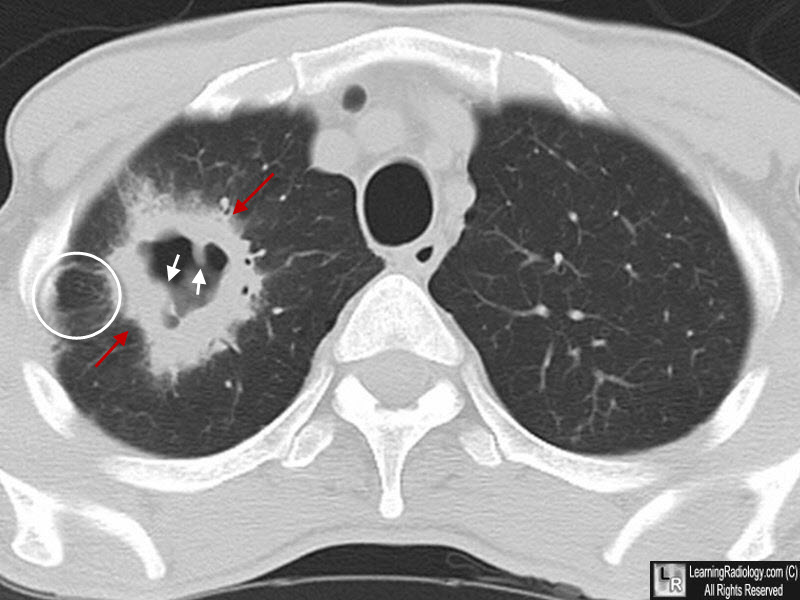
Cavitating Bronchogenic Carcinoma, Squamous Cell. There is a thick-walled cavity present in the right lung (red arrows) with spiculated outer margins (red arrows) and nodular inner margins (white arrows). There is associated lymphangitic spread (white circle. This was a squamous cell carcinoma, primary to the lung.
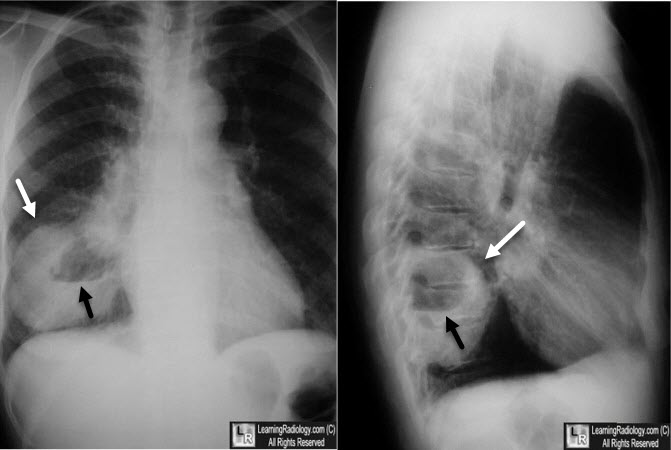
Cavitating Bronchogenic Carcinoma, Squamous Cell. There is a thick-walled cavity present in the right lower lobe (white arrows) with a nodular inner margin to the cavity. An air-fluid level is present. This was a squamous cell carcinoma, primary to the lung.
·
Adenocarcinoma
o
Usually
peripheral nodule
o
Found
in scars
o
Solitary
pulmonary nodule (52%)
o
Upper
lobe distribution (69%)
·
Small
cell undifferentiated=Oat Cell Carcinoma
o
Appearances
§
Mediastinal adenopathy
§
Hilar mass
§
Small or invisible lung nodule
o
High
metastatic potential
o
Rapid
growth
o
May
be associated with
§
Hypoglycemia
§
Cushing's syndrome
§
Inappropriate secretion of ADH
§
Excessive gonadotropin secretion
·
Large
cell undifferentiated (10%)
o
Large
peripheral mass
o
Pleural
involvement
·
Cell
type by location
o
Central
§
Squamous cell
o
Peripheral
§
Adenocarcinoma
§
Large cell
·
Most common site: anterior
segment RUL
o
Pancoast
tumor=superior sulcus tumor (4%)
o
Squamous
cell most often
o
SVC
obstruction (5%)
§
Most often small cell
·
Associated
clinical findings
o
Horner's
syndrome
§
Pancoast tumor
o
Elevated
hemidiaphragm
§
Phrenic nerve paralysis
o
Hoarseness
§
Recurrent laryngeal nerve
(left>right)
o
SVC
obstruction
§
Small cell ca
o
Pleural
effusion (10%)
o
Dysphagia
o
Enlarged
nodes
o
Esophageal
invasion
·
Roentgenographic
findings
o
Airway
obstruction
§
Atelectasis most common sign
§
No air bronchogram
§
Also postobstructive pneumonia
o
Hilar
enlargement
§
From either the carcinoma itself
or nodes
§
Particularly common in oat cell,
uncommon in adenoca
o
Mediastinal
node enlargement
§
Particularly anaplastic ca
o
Cavitation
§
Common (2-16%)
§
Especially in squamous cell,
mostly in upper lobes
§
Cavity is usually thick-walled
with nodular inner margin
o
Pleural
involvement
§
Common: 10%
§
Hemorrhagic effusion denotes
direct tumor invasion
§
Effusion carries a poor prognosis
even if no malignant cells are found
·
Metastases
o
Bone
§
Marrow: in 40% at time of
presentation
§
Gross lesions in 10-35%
§
Most often in vertebra (70%),
next in pelvis (40%), next femurs (25%)
§
Osteolytic mets (3/4)
§
Osteoblastic mets (1/4)
·
Especially in small cell and
alveolar cell
o
Adrenals
§
In 37% pathologically at time of
presentation
o
Brain
§
In 30% at autopsy
§
Multiple in 2/3
o
Kidney,
GI tract, liver, contralateral lung
·
Prognosis
o
Mean
survival time < 6 months
o
<10%
overall 5 year survival
o
Survival
by cell type at 40 months
§
Squamous cell (30%)
§
Large cell (16%)
§
Adenocarcinoma (15%)
§
Oat cell (1%)
|