
Collagen VascularDiseases
Collagen VascularDiseases

Collagen Vascular Diseases
Rheumatoid lung
Scleroderma
Lupus
Polyarteritis
Dermatomyositis/polymyositis
Goodpasture’s syndrome

Collagen Vascular Diseases
Common denominator is fibrinoidnecrosis of connective tissue
Thoracic structures involved about 2/3of all cases
All are immunologically-mediated

Rheumatoid Lung

Rheumatoid Lung
Extra-articular manifestations morecommon in males
Disease more common in females
Clinically
Shortness of breath most common
Subcutaneous rheumatoid nodules oftenpresent
PFTs show restrictive disease

Rheumatoid LungGeneral
Most patients with pulmonary evidenceof RA have
Clinical evidence of the disease
Severe arthritic disease

Circulating antibody
Largely IgM in patients with RA
Usually high titers of
Rheumatoid factor
Anti-nuclear antibodies
LE prep frequently positive
Rheumatoid Lung

Pleural effusion
Pulmonary fibrosis
Necrobiotic nodules
Caplan’s Syndrome
Pulmonary Arterial Hypertension
Obliterative Bronchiolitis
Rheumatoid LungSix manifestations

Most common manifestation of RA inchest
Exudate
Very low sugar content (< 30 mg/100 ml)
Does not rise with IV administration ofglucose
Low-sugar effusion in TB rises with IVglucose
Rheumatoid LungPleural Effusion

Pleural fluid in RA
Low sugar
High in LDH
Rich in lymphocytes
Positive for Rheumatoid Factor
Contains low complement levels
Low pH
Pleural EffusionCharacteristics

Effusion may remain unchanged formonths or years
Most are unilateral
Slightly more on right
Effusion almost never associated withparenchymal disease
Pleural EffusionCharacteristics

Rheumatoid Effusion

Type III immune rx (Arthus rx-IgG or IgM)
Begins micronodular or coarse reticulation
More prominent at bases
Indistinguishable from scleroderma
Honeycomb appearance
Thickened interlobular septa
Irregular pleural surfaces
Rheumatoid LungPulmonary Fibrosis

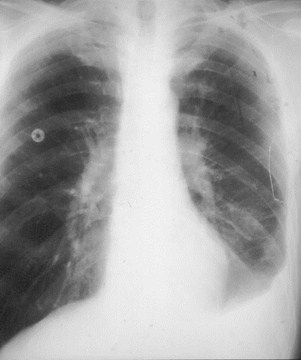
Pulmonary Fibrosis in Rheumatoid LungCoarse reticular

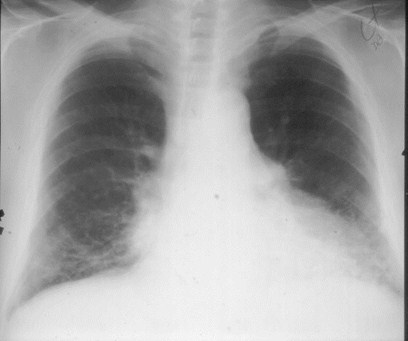
Pulmonary Fibrosis in Rheumatoid LungHoneycomb

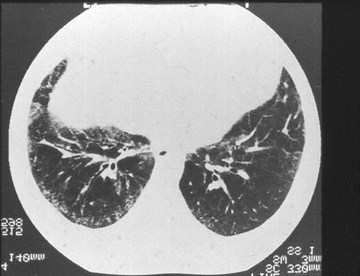
CT of Pulmonary Fibrosis in Rheumatoid Lung
Reticularopacities insubpleuralzones
Thickenedinterlobularsepta
Irregularpleuralsurfaces

Bibasilar Interstitial Disease
Bronchiectasis
Aspiration
DIP
Asbestosis
Sarcoidosis
Scleroderma


Pulmonary Fibrosis in Rheumatoid Lung

Relatively rare
Usually occur with subcutaneous nodules
Pathologically identical to them
Usually well-circumscribed masses
Typically multiple
Subpleural in location with cavitation
Frequently at bases
Rheumatoid LungNecrobiotic Nodules



Rheumatoid Nodule

Rheumatoid Nodule

R3
Rheumatoid Nodules

Necrobiotic nodules with silicosis
Roentgenographically identical torheumatoid nodules in RA
Pathologically, only difference is ringof dust in nodule which producesdarkened ring around central core
Rheumatoid LungCaplan’s Syndrome

Caplan’s SyndromeRheumatoid nodules and silicosis

Most often 2° pulmonary fibrosis
May be due to an arteritis PAH andeventual cor pulmonale
Findings are enlarged main, right andleft pulmonary arteries
Rheumatoid LungPulmonary Hypertension


R3
PAH 2° Rheumatoid Lung

Same as BOOP except patients have RA
Rheumatoid LungBOOP

Scleroderma

SclerodermaProgressive Systemic Sclerosis
90% of patients with disease have lungdisease
About 25% have abnormal chest x-rays
3:1 female to male ratio
Rheumatoid factor found in 35%
Increased incidence of lung cancer
Bronchoalveolar cell

Scleroderma3+ Thoracic Manifestations
Interstitial fibrosis
Pulmonary vascular disease (PAH)
Pleural changes (uncommon)
Recurrent aspiration
Calcinosis
Air esophagram
Air in dilated esophagus without fluid

SclerodermaX-ray Findings
Diffuse reticular interstitial disease
Primarily at bases
Fine coarse reticulation
Honeycombing
Alveolar infiltrates 2° aspiration
From disturbed esophageal motility

Scleroderma-Coarse with Honeycombing


SclerodermaX-ray Findings
Progressive volume loss
Unlike other causes of diffuse fibrosisexcept Hamman-Rich
Pleural disease rare
Unlike RA and lupus


SclerodermaOther Organs
GI tract
Esophageal dilatation
Small bowel dilatation
Pseudosacculations in colon
Resorption of terminal phalanges
Calcinosis circumscripta




CREST Syndrome
Benign variant of scleroderma
Calcinosis
Raynaud’s
Esophageal dysmotility
Sclerodactyly
Telangiectasia



Lupus Erythematosis

Systemic Lupus Erythematosus
Lungs and pleura involved more often inlupus than other collagen vasculardiseases
Prototype disease for Type III immunereaction (Arthus rx)

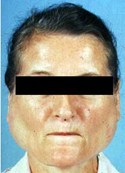
LupusClinical
Much more common in young women
Anti-nuclear antibody present in 87%
LE cells in 78%
Rheumatoid factor in 21%
False + test for syphilis in 24%

LupusClinical
Painful pleuritis with fever
Skin changes include
Butterfly rash
Alopecia
Photosensitivity
Raynaud's
Sjogren’s syndrome frequent


Lupus 6 Manifestations
Pleural effusions
Discoid atelectasis at both bases
Fleeting patchy infiltrates
Pericardial effusions
Lupus pneumonitis
Sluggish diaphragm
Not diffuse interstitial lung disease

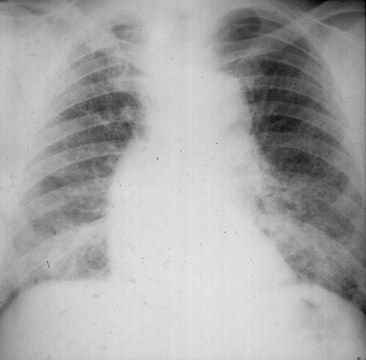
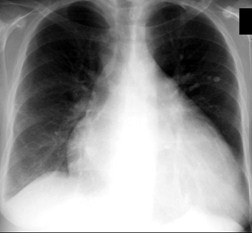
SLEPleural Effusions
Most common thoracic manifestation
Usually bilateral and small
If unilateral, more often on left
Exudates with
High protein
Normal glucose


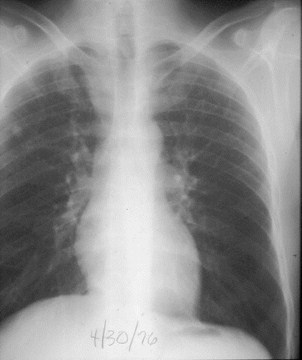
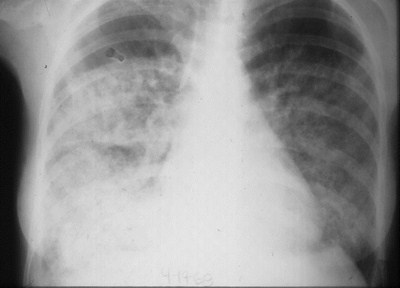
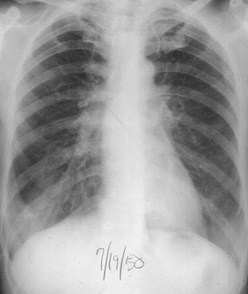
SLE with bilateral effusions


SLE with bilateral effusions


SLE with unilateral left effusion

SLEDiscoid Atelectasis
Horizontal lines
Basilar
Migratory and fleeting
Often associated with pleural effusion


R3
SLE with SSA

SLEPatchy Infiltrates
Usually at bases
Usually peripheral
Acute and fleeting
Small areas of pneumonitis
Cause unknown


R3
SLE with patchy RLL infiltrate

SLEPolyserositis
May have both pericardial and pleuraleffusions
Usually small

R3

SLE with Pericardial and Pleural Effusion

SLELupus Pneumonitis
Uncommon
2° vasculitis and hemorrhage
Severe dyspnea, fever and hypoxia
Responds to steroids or cytotoxic agents


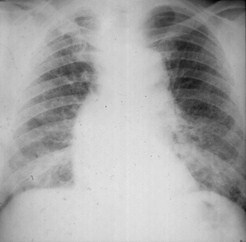
Lupus Pneumonitis

SLESluggish Diaphragm
Diffuse myopathy of diaphragmaticmuscles
Elevated hemidiaphragms
Loss of lung volume
Sluggish movement on fluoroscopy

Drug-induced Lupus
Hydralazine
Pronestyl (procainamide)
Dilantin
INH
Account for 90% of cases of drug-induced lupus

Drug-induced Lupus
Pleuroparenchymal changes morecommon than SLE
Does not involve kidney
More benign course
Disappears if drug is stopped

Polyarteritis Nodosa

Polyarteritis Nodosa
Affects small and medium-sized arterywalls with necrotizing granulomas in allwall layers

Polyarteritis NodosaGeneral
More common in adult males
Associated with hepatitis B antigen
Systemic hypertension common
Has much in common with Wegener'sgranulomatosis

Polyarteritis NodosaFindings
Findings variable & rarely characteristicenough to allow diagnosis
Most characteristic pattern is fleeting,patchy consolidation identical toLoeffler’s

Polyarteritis NodosaX-ray manifestations
Fleeting patchy infiltrates
Pericardial effusion
Pleural effusion
Discoid atelectasis
Nodules

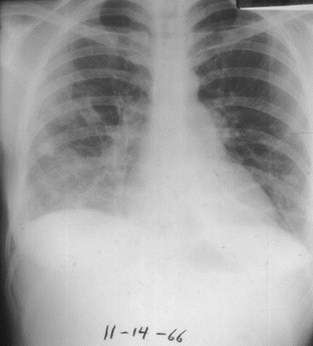
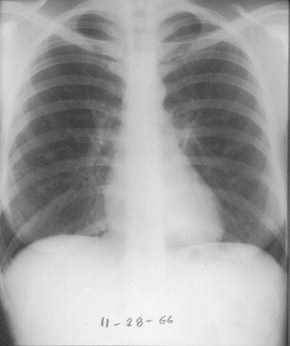
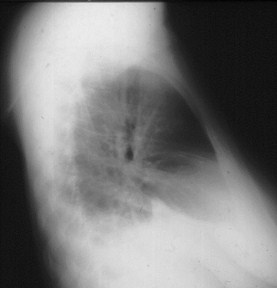
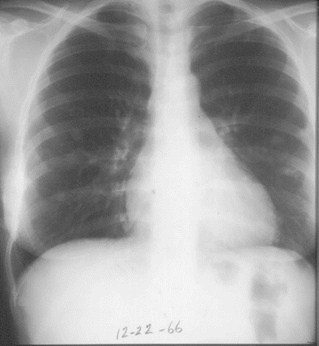
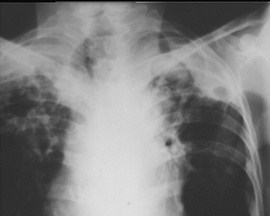
11/14
11/28
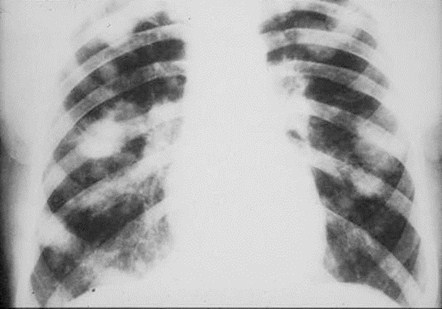
Polyarteritis nodosa with fleeting infiltrateand nodules

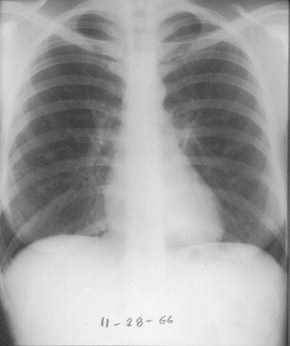
11/28
12/22
Polyarteritis nodosa with fleeting infiltrateand nodules

Polyarteritis NodosaFindings
Angiographic demonstration of multipleaneurysms in one or more abdominalorgans - especially the kidney - isdiagnostic of disease

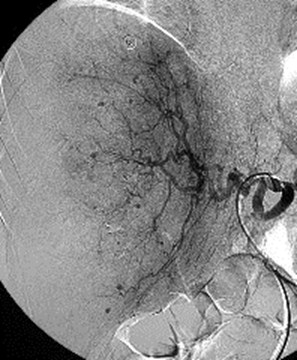
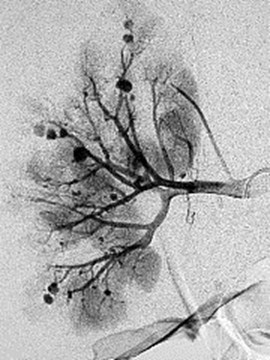
Kidney
Liver

Dermatomyositis
Polymyositis

Dermatomyositis
Weakness and pain in proximal limbmuscles
Violaceus rash
Sometimes neoplasms
Much more common in women
Two peaks: 1st then 5th decades
Unlike others, no circulating immunecomplexes


Chronic interstitial pneumonia
Aspiration pneumonia 2° esophagealdysmotility
Pneumonia 2° chest-wall involvement
Dermatomyositis3 manifestations

Diffuse reticular opacities
Primarily at bases
Aspiration pneumonia
Calcinosis universalis
More often in children
DermatomyositisX-ray manifestations


Ankylosing Spondylitis
Upper lobe fibrotic and bullous disease

Goodpasture’sSyndrome

Idiopathic Pulmonary HemorrhageGoodpasture’s Syndrome
Both characterized by repeatedepisodes of pulmonary hemorrhage
Both produce iron-deficiency anemia
Both can produce pulmonaryinsufficiency

Pathology
Hemorrhage typically confined toperipheral airspaces
Diffuse interstitial fibrosis, hemosiderosiscommon
Vasculitis not always present even thoughthese are autoimmune diseases

Idiopathic Pulmonary HemorrhageGoodpasture’s Syndrome
Prognosis for both diseases grave –both treated with steroids andcytotoxic agents

Goodpasture’s syndrome
Disease of young adults
Most are men
Goodpasture’s includes renal disease
Renal lesion=glomerulonephritis
Autoimmune etiology
Both lung and renal pathology believed 2°to anti-glomerular basement membraneantibody cross reacting with lung basementmembrane

Goodpasture’s syndromeNatural History
Early disease alveolar in nature
More prominent at the bases and perihilarregions — simulates pulmonary edema
Within 2-3 days, blood absorbed intointerstitium
Pattern changes to reticular interstitial

Goodpasture’s syndromeNatural History
By about 10 days, reticular diseasedisappears
With repeated bleeds, there ishemosiderin deposit in the lungs andprogressive pulmonary fibrosis occurs

Goodpasture’s syndromeNatural History
Once this occurs, new hemorrhagesuperimposed on old interstitialdisease
Reticular pattern remains rather thandisappears when blood is absorbed

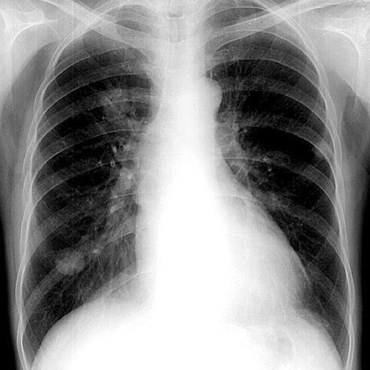
Goodpasture’s SyndromeAcute hemorrhage

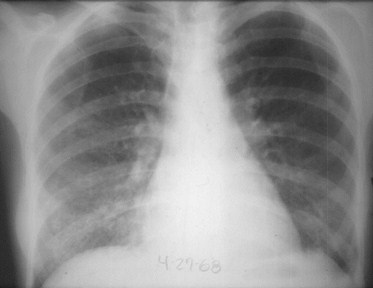
Goodpasture’s SyndromeRapid clearing

Goodpasture’s syndromeOther Findings
May have pulmonary hypertension
May have hilar adenopathy

Take Home Points


Rheumatoid Lung

Pleural effusions
Pulmonary fibrosis
Necrobiotic nodules
Low sugar
Clinical disease present
Eroded clavicles

Scleroderma

Interstitial fibrosis
No pleural disease
Aspiration pneumonia
Air esophagram
Alveolar cell ca


Lupus

Pleural effusions
Discoid atelectasis
Patchy infiltrates at thebases
No diffuse interstitial lungdz
Drug-induced morecommon and benign


Polyarteritis

Fleeting patchyinfiltrates
Aneurysms of smallvessels of kidney andliver

Dermatomyositis

Calcinosis universalis
Interstitial lung dz
Aspiration pneumonia
Higher incidence ofcolorectal ca


Goodpasture’s

Repeatedhemorrhages into lung
Lead to pulmonaryfibrosis
Glomerulonephritis


The End