
Pneumonia
All copyrighted material retains the rights of the original authors
© William Herring, MD, FACR

Gram PositivePneumonias

Gram Positive Pneumonias
Pneumococcal pneumonia
Staphylococcal pneumonia
Streptococcal pneumonia
Nocardiosis

Pneumococcal PneumoniaGeneral
Most common gram positive pneumonia
90% community acquired
Organism: strep pneumoniae
Inflammatory edema in alveoli spread viapores of Kohn to more lateral alveoli

Pneumococcal PneumoniaPredisposing Conditions
Usually found in compromised hosts
Elderly
Type 3 especially fatal to elderly
Debilitated, sicklers
Most often types 8, 4, 5 and 12

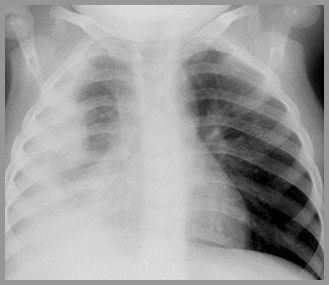
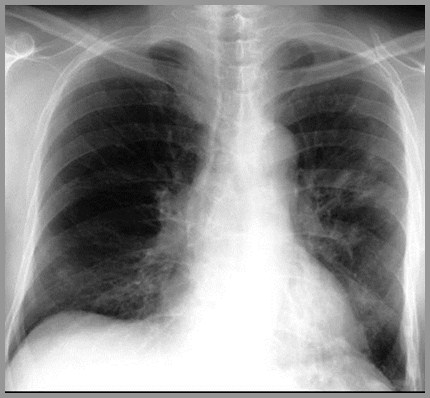
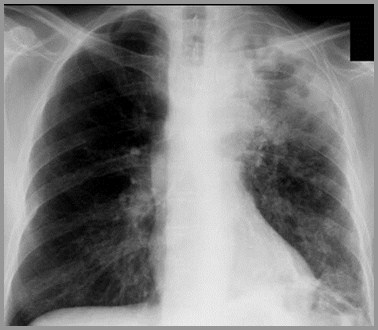
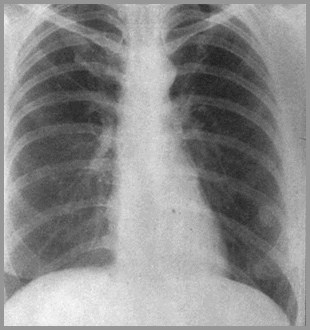
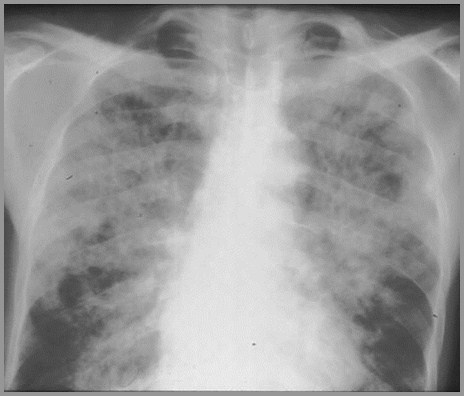
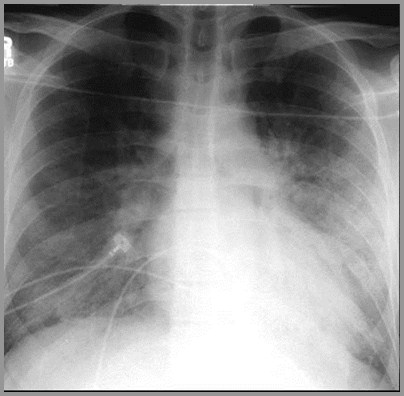
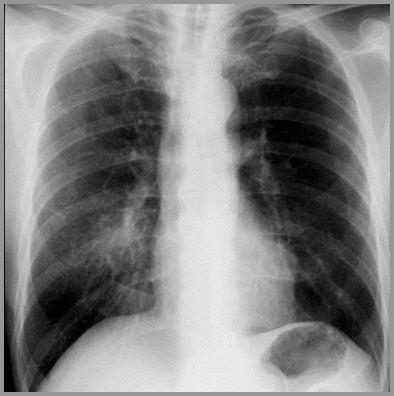
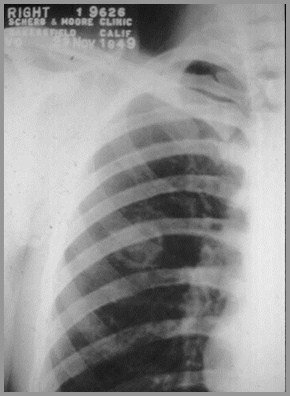
Pneumococcal PneumoniaX-ray Findings
Organism aspirated into lungs
Predilection for lower lobes
Extensive infiltrate abutting pleural surface
Prominent air bronchograms
DDX: Staph has no air bronchogram
Does not respect segmental boundaries

Pneumococcal pneumonia
© R3

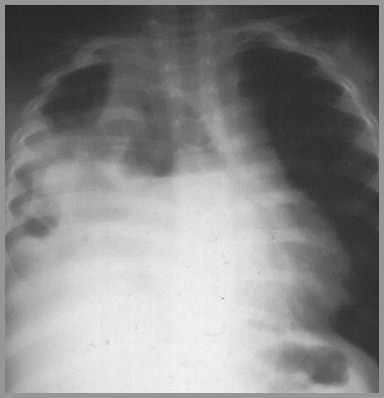
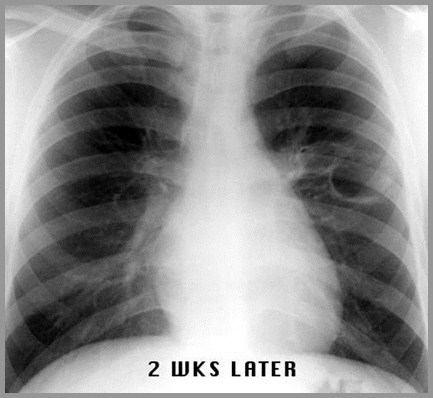
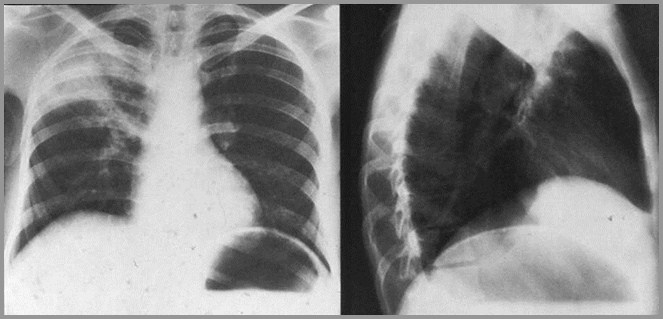
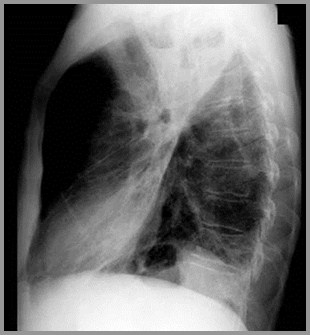
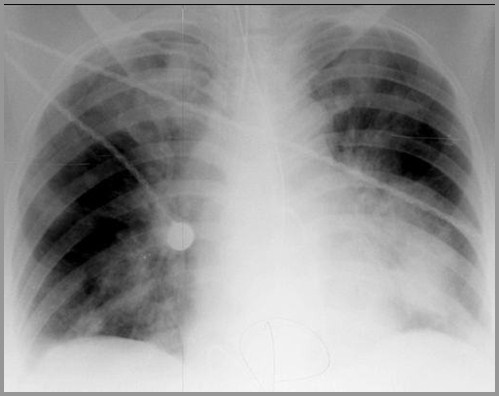
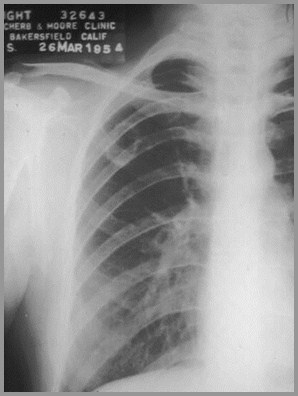
Pneumococcal PneumoniaResolution
Resolution begins promptly with antibiotics
Frequently within 24 hours

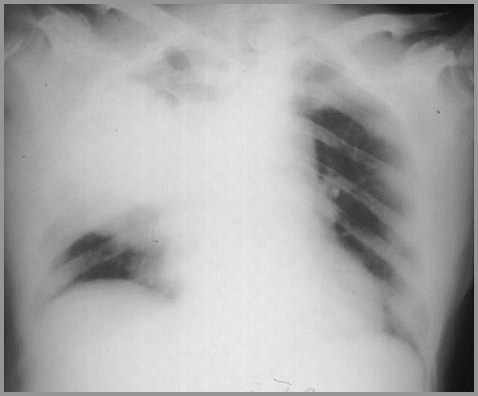
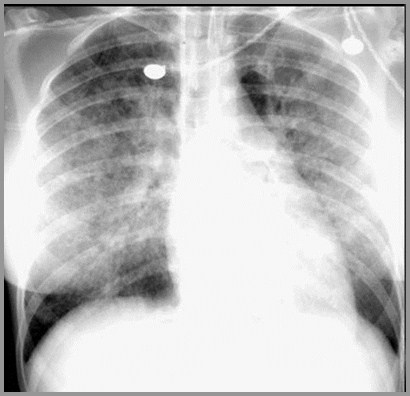
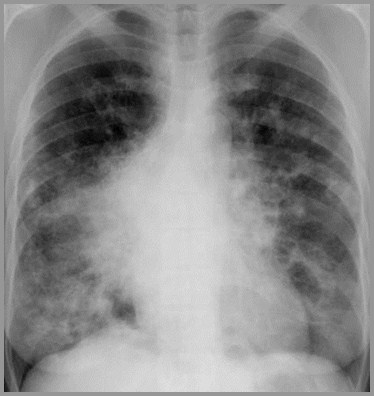
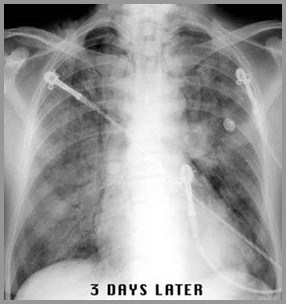
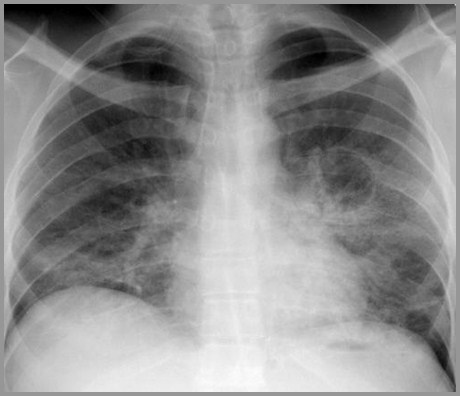
Rapidly Clearing Alveolar Infiltrate
1.Pneumococcal pneumonia
2.Hemorrhage
3.Pulmonary edema
4.Aspiration
DDX

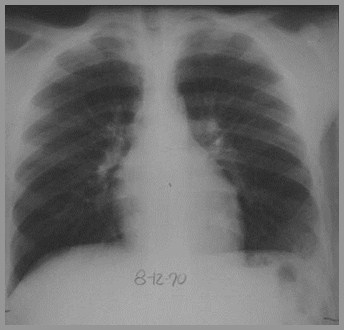
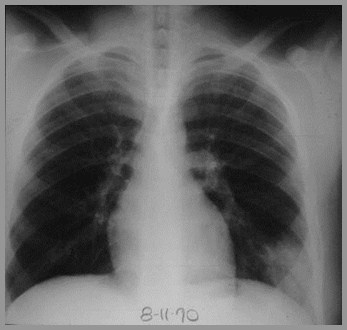
Day 1
Day 2
Rapid Clearing

Staph Pneumonia

Staph Aureus PneumoniaGeneral
Most common bronchopneumonia
Overwhelming majority hospital-acquired
Rarely develops in healthy adults
Most common cause of death duringinfluenza epidemics

Produces pathologic reaction inconducting airways
Hemolyzes blood agar, coagulasepositive
Pathology in humans due to production ofcoagulase
Staph Aureus PneumoniaGeneral

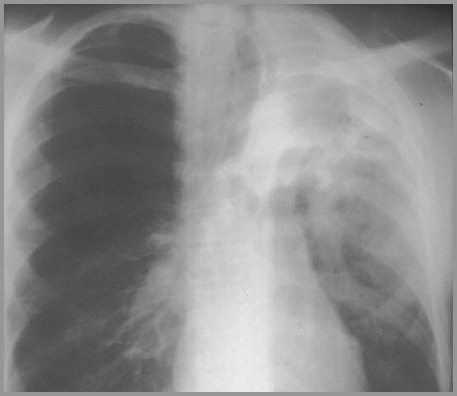
Staph Aureus PneumoniaX-ray
Rapid spread through lungs
Empyema, especially in children
No air bronchogram
Pneumothorax, pyopneumothorax
Abscess formation, pneumatocoele
Bronchopleural fistula

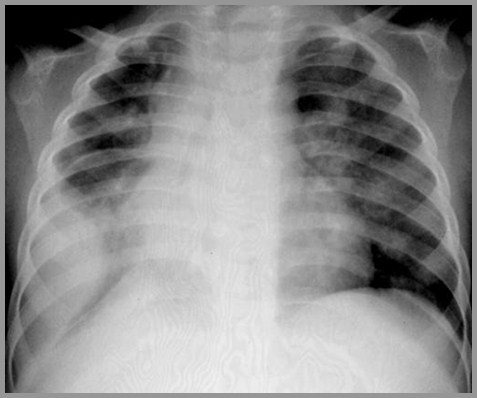
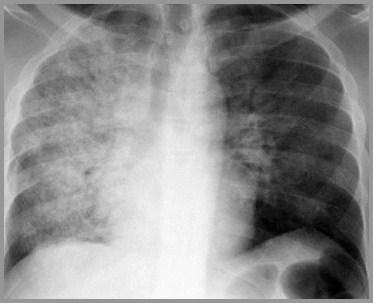
Infiltrates with Effusion
1.Staph pneumonia
2.Strep pneumonia
3.TB
4.Pulmonary infarct
DDX

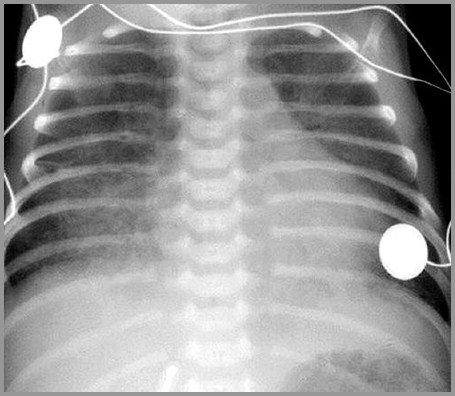
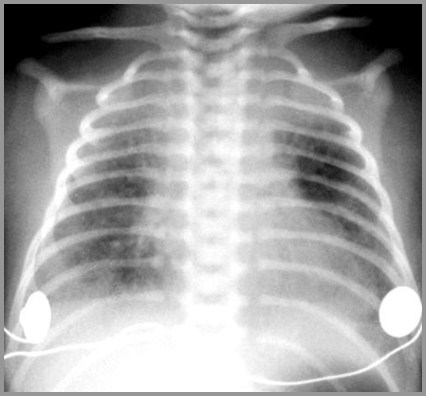
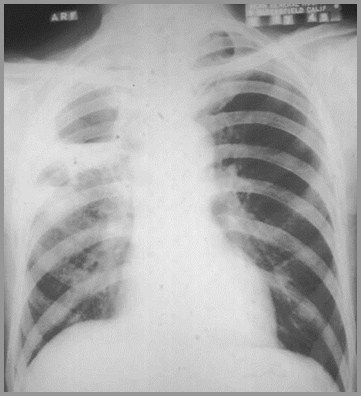
Staph Aureus PneumoniaAppearance In Children
Rapidly developinglobar/multilobar consolidation
Pleural effusion (90%)
Pneumatocoele

Staph pneumonia
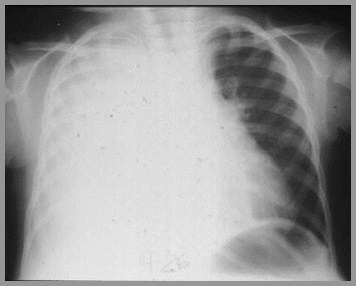
Day 1
Day 4

Staph pneumonia with cavitation

Staph pneumonia with pneumatocoele

Staph pneumonia with empyema

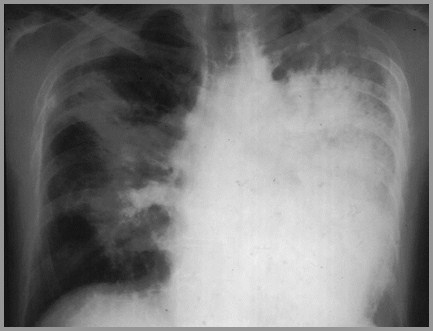
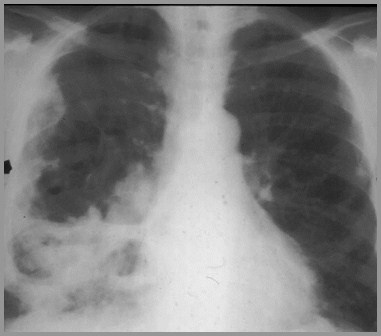
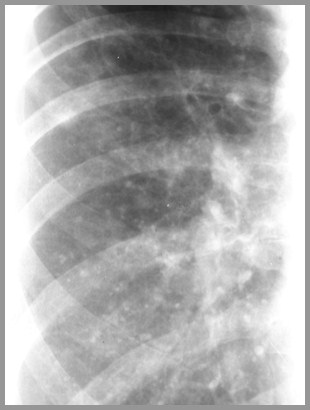
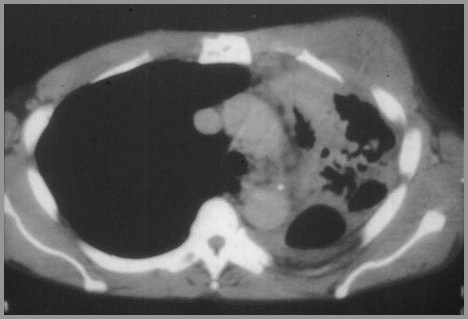
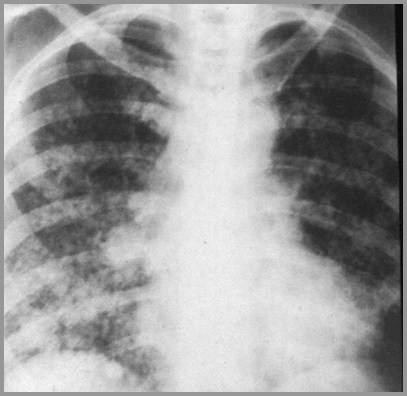
Staph Aureus PneumoniaAppearance In Adults
Patchy bronchopneumonia, segmentaldistribution
Frequently bilateral
May be associated with atelectasis sinceairways are filled
Not so with pneumococcal
Pleural effusion (50%)

Staph pneumonia
© R3

Staph pneumonia with atelectasis
© Gower

Strep Pneumonia

Streptococcus PyrogenesPneumonia
Most common in winter
Only 5% of bacterial pneumonias
Group A Beta hemolytic strep
Predisposed
Newborns and following measles

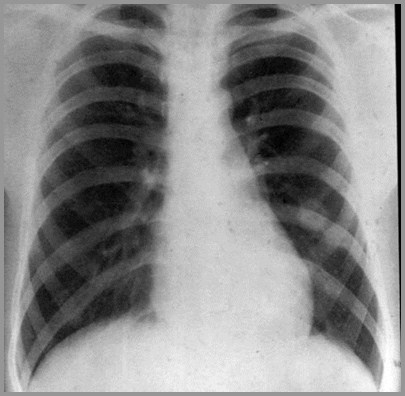
Streptococcal PneumoniaX-ray Findings
Looks like staph pneumonia
Less tendency to producepneumatocoeles
Almost always lower lobes
Patchy bronchopneumonia
Empyemas do form

Strep pneumonia
© R3

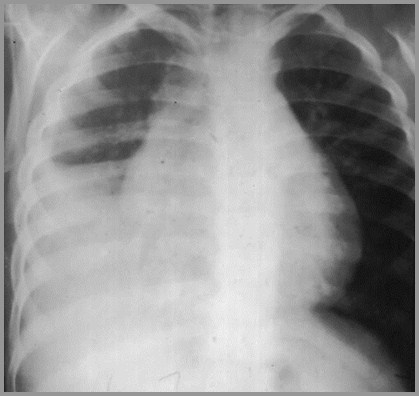
Strep pneumonia

Strep pneumonia in newborn
© R3

Streptococcal PneumoniaComplications and Associations
Complications
Bronchiectasis
Lung abscess
Glomerulonephritis
Associated with
Delayed onset of diaphragmatic herniasin newborns

Nocardiosis

Nocardiosis
Gram-positive, acid-fast bacterium
Occurs in immunocompromised
Multiple nodules with or withoutcavitation
Empyemas occur

Nocardiosis – nodules with cavitation

© R3

Gram NegativePneumonias

Gram Negative Pneumonias
Pseudomonas
Klebsiella
Enterobacter
Serratia
Anaerobic

Pseudomonas AeruginosaGeneral
Gram negative rod
Frequently hospital-acquired
Frequently related to inhalators ornebulizers
Many patients on multiple antibiotics and/orsteroids

Pseudomonas AeruginosaPredisposed
COPD
CHF
Alcoholism
Kidney disease
Those with trachs

Pseudomonas AeruginosaX-ray Findings
Resembles staph pneumonia
Predilection for lower lobes
Usually affects both lungs
Contains multiple small lucencies
Lung abscess > 2 cm may also occur
Widespread nodular shadows anothermanifestation


Pseudomonas pneumonia with multiple cysticlucencies

Pseudomonas


Pseudomonas lung abscess

Cavitating Pneumonia
1.Staph
2.Strep
3.TB
4.Gram negative pneumonia
DDX

Pseudomonas lung abscess

Klebsiella, Enterobacter, SerratiaGeneral
Encapsulated, gram negative rods
Most are hospital-acquired
Most occur in chronic alcoholics
Aspirated into lungs
Most are unilateral and right sided

Klebsiella PneumoniaX-ray Findings
Produces excessive amounts ofinflammatory exudate
Affected lung gains volume and fissures bulge
Bulging fissure sign
Abscess and cavity formation common
Pleural effusion and empyema common

Klebsiella with bulging fissure

Cavitating Klebsiella pneumonia
© R3

Klebsiella PneumoniaX-ray Findings
May result in gangrene of lung
Massive pieces of lung tissue fall intoan abscess cavity
Serratia marcescens may causebronchopneumonia

Anaerobic OrganismsGeneral
Frequently from aspiration of gastriccontents
Organisms include:
Bacteroides melaninogenicus
B. fragilis

Anaerobic OrganismsX-ray Findings
Almost always lower lobes
Frequently right-sided
Homogeneous consolidation
About 70% have pleural involvement–effusion, empyema
May progress very rapidly
Half develop abscesses

Anaerobic lower lobe cavitary pneumonia

Anaerobic pneumonia with effusion

Other Pneumonias

Other Pneumonias
Cryptococcus
Varicella
Pneumocystis
Actinomycosis
Mycoplasma pneumonia
Coccidiomycosis

Cryptococcosis

Cryptococcosis(Torulosis)
Caused by Cryptococcus neoformans
Found in soil contaminated with pigeonexcrement
Granulomatous disease
Diabetics, immunocompromised
Frequently produces meningitis

CryptococcosisX-ray
Well circumscribed peripheral mass (40%)
Lobar/segmental consolidation (35%)
Cavitation (15%)
Hilar/ mediastinal adenopathy

Cryptococcal nodule

Varicella Pneumonia

Varicella PneumoniaGeneral
Occurs most often > 19 years old
Associated with vesicular rash
11% mortality rate

Varicella PneumoniaX-ray Findings
Patchy, diffuse air space consolidation
Tendency to coalesce near hila
Widespread nodules can occur (30%)
Tiny calcifications remain in 2%
DDX:histoplasmosis, alveolar microlithiasis

Acute Varicella pneumonia
© R3

Chronic Varicella with multiple calcifications

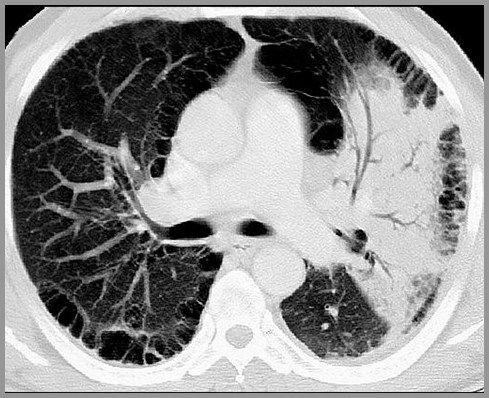
Pneumocystis CariniiPneumoniaPCP

Pneumocystis PneumoniaGeneral
Fungus pneumocystis carinii
Most common cause of pneumonia inimmunocompromised hosts
Often associated with CMV, herpessimplex, MAI
Lymphopenia foretells poor prognosis

Pneumocystis PneumoniaX-ray
Most often central location, reticularinfiltrate
Resembles pulmonary edema
Pleural effusion uncommon
Hilar adenopathy does not occur
Gallium taken up prior to x-ray changes

PCP

PCP mimicking CHF

PCP
© R3

PCP
© R3
Two different patients

PCP
© R3

Pneumocystis PneumoniaAssociated Findings
May be associated with nodules
Kaposi’s, lymphoma, septic emboli
Cavities may occur
Superimposed fungal, mycobacterialinfection
Bullae and thin walled cysts (38%)
Pneumothorax (18%)

PCP with pneumatocoele formation
© R3

Actinomycosis

ActinomycosisGeneral
Actinomyces israeli, gram+ pleomorphicanaerobic bacterium
Related to the morphology of fungus andMycobacterium—not acid fast
Once was most common pulmonaryfungal disease
White or yellow “sulfur granules”
Really mycelial clumps

ActinomycosisContinued
Rod shaped form found “normally” indental caries, gingival margins, tonsillarcrypts and GI tract
Predisposed: poor dental hygiene andimmunosuppressed
Affects mandibulofacial area, intestinaltract and lung, in that order

Mandibulofacial Actinomycosis
Osteomyelitis of mandible — with softtissue mass – “lumpy jaw”

Intestinal Actinomycosis
Resembles Crohn’s disease
May produce rupture of hollowviscus, especially appendix
May produce fistula formation

Pulmonary ActinomycosisX-ray Findings
Consolidation which extends acrossfissure — peripheral and lower lobe
DDX for lung consolidation which extendsthrough chest wall:
Blastomycosis
TB
Crytococcosis

Pulmonary ActinomycosisX-ray Findings–Continued
Abscess
Empyema
Osteomyelitis of the rib
Wavy periosteal reaction, rarely ribdestruction
Draining chest wall sinuses
If chronic, it results in severe fibrosis

Actinomycosis

Actinomycosis extends from lung through pleura

MycoplasmaPneumoniaMycoplasmaPneumonia
Primary atypical pneumoniaPrimary atypical pneumonia

Mycoplasma PneumoniaPrimary atypical pneumonia
Commonest cause of nonbacterial pneumonia
Mild course
Lasts 2-3 weeks
Peak in autumn and winter
Common
1/3 of all pneumonias in service personnel
Organism: Eaton agent=pleuropneumonia-likeorganism (PPLO) – probably a bacterium

Mycoplasma PneumoniaClinical
One group has acute onset of fever, cough,chest pain with segmental pneumonia
Other group has 1-4 week history of lethargyand SOB usually with interstitial disease
May have bullous myringitis
Cultures take 3 months so 4X rise in coldagglutinins is used in diagnosis

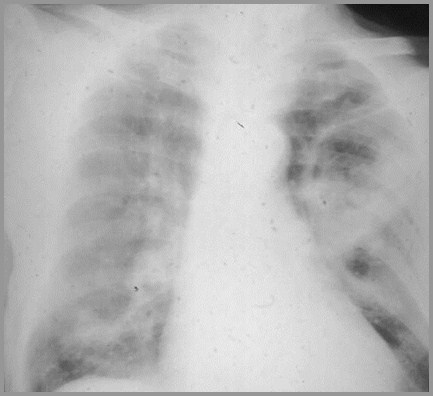
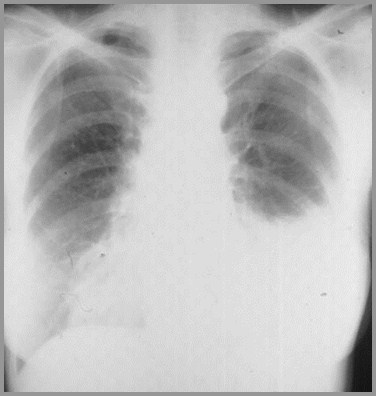
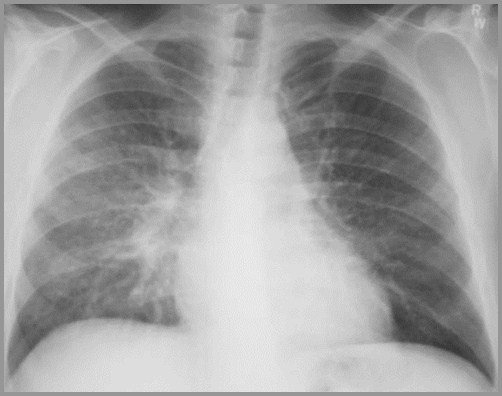
Mycoplasma PneumoniaX-ray Findings
Acute interstitial infiltrate
Lower lobes radiating from hila (early)
Then alveolar infiltrates
Usually unilateral and almost alwayssegmental
Small pleural effusion in 20%
Rare hilar adenopathy

Mycoplasma pneumonia
© R3

Mycoplasma pneumonia with B/L infiltrates
© R3


© Gower
Mycoplasma pneumonia with B/L infiltrates

Mycoplasma PneumoniaComplications
Meningitis
Encephalitis
Stevens-Johnson Syndrome
Erythema multiforme
High fever
Stomatitis
Pneumonia
Erythema nodosum

Coccidioidomycosis

Coccidioidomycosis
Caused by Coccidioides imitus
Soil fungus endemic to Southwest (SanJoaquin Valley)

Primary Coccidioidomycosis
Most are asymptomatic
Clinically, may have arthralgias, skinrash
X-ray
Patchy infiltrates mainly in lower lobes(80%)
Hilar adenopathy (20%)
Pleural effusion (10%)

DisseminatedCoccidioidomycosis
Meningeal spread
Micronodular lung pattern

Coccidiomycosis
© Gower

Chronic Coccidioidomycosis
One or more well-defined nodules(5%)
“Grape-skin” thin-walled, upper lobecavity
Mostly solitary
Resembles TB
Mediastinal adenopathy (10%)

Chronic Coccidiomycosis - nodule
© Gower

Chronic Coccidiomycosis

Chronic Coccidiomycosis-thin-walled cavity

Coccidiomycosis

Nodular Infectious Diseases
1.Nocardiosis
2.Coccidiomycosis
3.Cryptococcosis
4.Varicella

Take Home Points
Pneumococcal pneumonia can clear in48 hrs
Staph produces loculated effusions andpneumatocoeles
Nocardiosis has multiple nodules withor without cavitation



Take Home Points
Pseudomonas - lower lobes; multiplesmall lucencies
Klebsiella - heavy exudate; bulgingfissure
Actinomycosis – extends throughpleura



Take Home Points
Mycoplasma – lower lobe; dormitorysettings
Coccidiomycosis – thin-walled cavity



The End