- Presence of air in the pleural space
- Anatomy
- Visceral pleura is adherent to lung surface
- There is no air in the pleural space normally
- The introduction of air into the pleural space separates the visceral from the parietal pleura
- In contradistinction, the visceral and parietal pleura usually do not separate from each other in obstructive atelectasis
- Pathophysiology
- Either from disruption of visceral pleura
- Or, trauma to parietal pleura
- Clinical findings
- Acute onset of
- Pleuritic chest pain
- Dyspnea (in 80-90%)
- Cough
- Back or shoulder pain
- Etiologies
- Penetrating trauma
- Blunt trauma
- May be due to rib fracture
- May be caused by increased intrathoracic pressure
- May lead to bronchial rupture
- “Fallen lung sign” (ptotic lung sign) -- hilum of lung is below expected level within chest cavity
- Persistent pneumothorax with functioning chest tube
- Iatrogenic
- Tracheostomy
- Central venous catheter attempt or insertion
- Mechanical ventilation
- May occur in up to 25% of patients maintained on PEEP
- May be bilateral or under tension
- Thoracic irradiation
- Spontaneous pneumothorax
- Most common etiology
- Cause
- Rupture of subpleural blebs in apical region of lung
- Age
- 20-40 years
- M:F = 8:1
- Especially in patients who are tall and thin
- Smokers
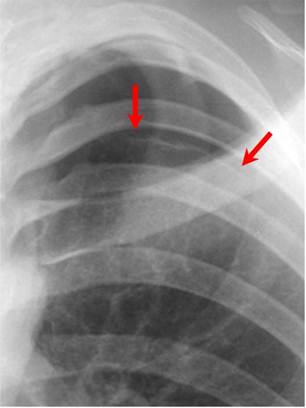
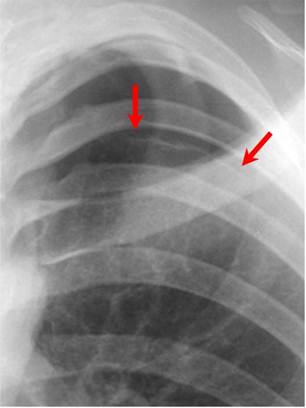
Red arrows point to thin white visceral pleural line which
is the single best sign for a pneumothorax
- Prognosis
- Recurrence in 30% on same side
- Recurrence in 10% on contralateral side
- Treatment
- Simple aspiration (success in >50%)
- Tube thoracostomy (effective in 90%)
- Other causes of a pneumothorax
- Neonatal disease
- Meconium aspiration
- Respirator therapy for hyaline membrane disease
- Malignancy
- Primary lung cancer
- Lung metastases, especially from osteosarcoma
- Also pancreas, adrenal, Wilms tumor
- Pulmonary infections
- Tuberculosis
- Necrotizing pneumonia
- Coccidioidomycosis
- Hydatid disease
- Pertussis
- Acute bacterial pneumonia
- Staphylococcal septicemia
- AIDS (Pneumocystis carinii, Mycobacterium tuberculosis, atypical mycobacteria)
- Complication of pulmonary fibrosis
- Histiocytosis X
- Idiopathic
- Cystic fibrosis
- Sarcoidosis
- Scleroderma
- Eosinophilic granuloma
- Interstitial pneumonitis
- Rheumatoid lung
- Idiopathic pulmonary hemosiderosis
- Pulmonary alveolar proteinosis
- Biliary cirrhosis
- Asthma or emphysema
- Produce a second peak incidence of pneumothorax from 45-65 years of age
- Due to rupture of peripheral emphysematous areas
- “Catamenial pneumothorax” is a recurrent spontaneous pneumothorax that occurs during menstruation and is associated with endometriosis of the diaphragm
- Marfan’s syndrome
- Ehlers-Danlos syndrome
- Pulmonary infarction
- Lymphangiomyomatosis and tuberous sclerosis
- Incidence of pneumothorax is particularly high in lymphangiomyomatosis and histiocytosis X
- Types of pneumothorax
- Closed pneumothorax = intact thoracic cage
- Open pneumothorax = "sucking" chest wound
- Tension pneumothorax
- Accumulation of air within pleural space due to free ingress and limited egress of air
- Pathophysiology:
- Intrapleural pressure exceeds atmospheric pressure in lung during expiration (check-valve mechanism)
- Frequency
- In 3-5% of patients with spontaneous pneumothorax
- Higher in barotrauma (mechanical ventilation)
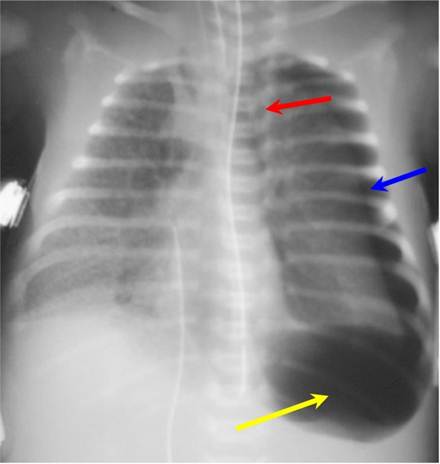
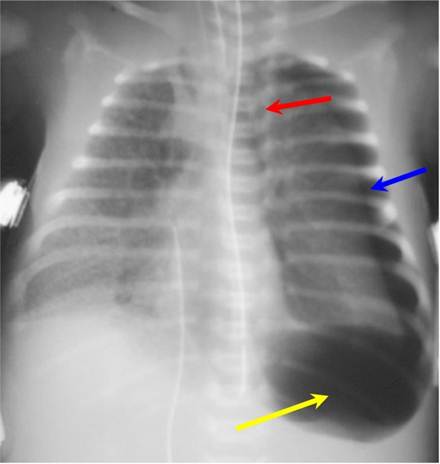
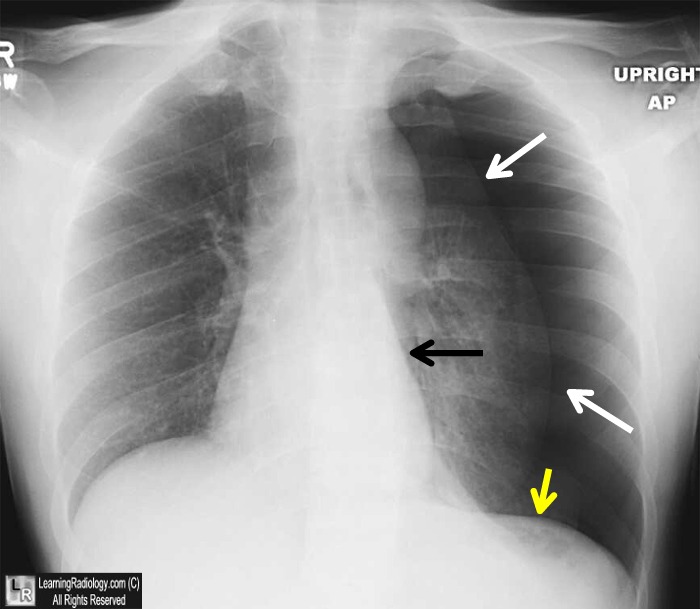
Tension pneumothorax on left (blue arrow) is displacing the heart and mediastinal structures to the right (red arrow);
this case also shows a deep sulcus sign on the left (yellow arrow). There is underlying hyaline membrane disease.
- Simple pneumothorax –no shift of the heart or mediastinal structures
- Imaging findings in pneumothorax
- Must see the visceral pleural white line
- Very thin white line that differs from a skin fold by its thickness
- Absence of lung markings distal or peripheral to the visceral pleural white line
- Not evidence enough to say there is a pneumothorax only if there are no lung markings seen
- No lung markings will be seen with bullous disease
- Bullae have a concave surface facing the chest wall
- Pneumothorax almost always has a convex surface facing the chest wall
- Displacement of mediastinum and/or anterior junction line
- Deep sulcus sign
- On frontal view, larger lateral costodiaphragmatic recess than on opposite side
- Diaphragm may be inverted on side with deep sulcus
- Total / subtotal lung collapse
- This is passive or compressive atelectasis
- Collapse of SVC or IVC due to decreased systemic venous return and decreased cardiac output
- Tension hydropneumothorax
- Sharp delineation of visceral pleural by dense pleural space
- Mediastinal shift to opposite side
- Air-fluid level in pleural space on erect chest radiograph
- Radiographic signs in upright position
- White margin of visceral pleura separated from parietal pleura
- Usually seen in the apex of the lung
- Absence of vascular markings beyond visceral pleural margin
- May be accentuated by an expiratory film in which lung volume is reduced while amount of air in pneumothorax remains constant so that relative size of pneumothorax appears to increase
- Radiographic signs in supine position
- Anteromedial pneumothorax (earliest location)
- Outline of medial diaphragm under cardiac silhouette
- Deep sulcus sign
- Decubitus views of the chest may demonstrate a pneumothorax on the side that is non-dependent
- Left lateral decubitus view for right-sided pneumothorax
- Right lateral decubitus view for left-sided pneumothorax
- Subpulmonic pneumothorax (second most common location)
- Hyperlucent upper abdominal quadrant
- Deep lateral costophrenic sulcus
- Sharply outlined diaphragm in spite of parenchymal disease
- Visualization of anterior costophrenic sulcus
- Visualization of inferior surface of lung
- Apicolateral pneumothorax (least common location)
- Visualization of visceral pleural line
- Posteromedial pneumothorax (in presence of lower lobe collapse)
- Lucent triangle with vertex at hilum
- V-shaped base delineating costovertebral sulcus
- Pneumothorax outlines pulmonary ligament
- Pitfalls in diagnosis
- Skin fold
- Thicker than the thin visceral pleural white line
- Air trapped between chest wall and arm
- Will be seen as a lucency rather than a visceral pleural white line
- Edge of scapula
- Follow contour of scapula to make sure it does not project over chest
- Overlying sheets
- Usually will extend beyond the confines of the lung
- Hair braids
- Prognosis
- Resorption of pneumothorax occurs at a rate of 1.25% per day (accelerated by increasing inspired oxygen concentrations)
|