|
|
Fracture of the Patella
Patellar Fracture
General Considerations
- The patella is the body’s largest sesamoid and lies in the quadriceps tendon
- Upper pole is site of attachment of the quadriceps tendon
- This tendon is comprised of components from the
- Superficial rectus femoris
- Vastus intermedius muscle
- Vastus medialis and lateralis
- Lower pole is the site of attachment of the patellar ligament which inserts at the tibial tubercle
- Portions of the rectus femoris course over surface of patella
- Normal position of the patella
- The inferior border is about the height of one patella above the knee joint space with the knee slightly flexed
Mechanism and Types
- Usually the result of a fall onto the knee or knee striking dashboard of automobile
- More frequently comminuted than indirect
- Less frequently has displaced fragments
- More frequent injury to articular cartilage
- Indirect mechanisms may include avulsion secondary to jumping or unexpected rapid flexion
- Less often comminuted than direct
- More often transverse, displaced or distracted
- Less often injury to articular cartilage
- Most injuries involve a combination of the two mechanisms
- Most fractures are transverse (medial to lateral)
- Vertical fractures (superior to inferior) are rare
- Osteochondral sleeve fractures

- More common in children and adolescents
- Results usually from forceful jumping
- Avulsion of any part of the articular surface, usually inferior pole
- Damage to articular cartilage also occurs
- Superior pole of patella may be high-riding
- Patellar fractures can also occur following surgery for anterior cruciate repair
Clinical Findings
- History of direct or indirect injury
- Pain, often severe
- Tenderness
- Limitation of motion
Imaging Findings
- Conventional radiography is the imaging study of first choice
- Lateral view should demonstrate most fractures
- Axial (skyline, sunrise) may show vertical fractures best
- Osteochondral sleeve fractures show avulsion of the inferior pole of the patella
- If the x-ray beam is oriented horizontally and image is obtained cross-table, a fat-fluid level (lipohemarthrosis) may be present

- CT is used when a fracture is suspected but not visible
- MRI can show bone contusions and muscular and tendinous injuries
- Better at characterizing cartilage injuries
Differential Diagnosis
- About 2% of population (9:1 males:females) have two un-united centers of ossification – the bipartite patella

- The un-united center is almost always in the upper outer quadrant of the patella
- Only about half (57%) of bipartite patellae are bilateral
Treatment
- Non-displaced fractures with less than 2 mm of step-off can be treated with immobilization with knee in extension for 4-6 weeks
- Displaced fractures with > 2 mm of step-off or 3 mm of distraction are treated surgically
- Common technique involves insertion of two Kirschner wires and a looped wire
- Partial or total patellectomy may be used for severe comminution
Complications
- Sepsis
- Mal- or nonunion
- Distraction of > 3 mm may lead to malunion or secondary osteoarthritis
- Avascular necrosis
- Part of blood supply enters from inferior pole
- Osteoarthritis of femoropatellar compartment
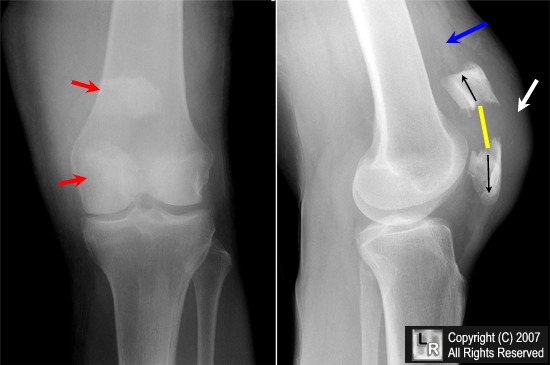
Patellar fracture. Frontal and lateral radiographs of the patella demonstrate a transverse fracture through the midpole of the patella with displacement of the superior pole (red arrow) by the quadriceps tendon and displacement of the inferior pole (red arrow) by the patellar tendon (black arrows). The result is marked distraction of the fragments (yellow line). There is soft tissue swelling (white arrow) and a joint effusion (blue arrow).
For additional information about this disease, click on this icon if seen above.
For this same photo without the arrows, click here
eMedicine Fractures, patella Christine Lamoureux, MD with Ray F Kilcoyne, MD
|
|
|