|
|
Pericardial Effusion
General Considerations
- Abnormal amount of fluid in the pericardial space, defined as the space between the visceral and parietal layers of the pericardium
- Normally contains about 20-50 cc of fluid
- Fat covers outside of heart and outside of pericardium sandwiching pericardial space between the two layers
- Normal thickness of pericardium (parietal pericardium and fluid in space) is 2-4 mm
Clinical Findings
- Small effusions frequently produce no symptoms
- Chest pain or discomfort with a characteristic of being relieved by sitting up or leaning forward and worsened in the supine position\
- Syncope
- Palpitations
- Shortness of breath, tachypnea
- Muffled or distant heart sounds, tachycardia
- Hypotension
- Jugular venous distension
- Pulsus paradoxus
- Decrease in systolic pressure with inspiration of more than 10 mm Hg
- Rate of accumulation of fluid is proportional to severity of symptoms
- The faster the fluid accumulates, the more severe the symptoms
- Requires about 150-250cc before cardiac tamponade occurs
- About 7-10% of those with pericardial effusion are at risk for developing tamponade
- Tamponade compresses heart and causes low cardiac output
- Most effusions do not lead to cardiac tamponade
- Size of cardiac silhouette is frequently increased
- Tamponade is rarely seen in association with pulmonary edema in the lungs
Causes
Causes of Pericardial Effusions |
Cause |
Remarks |
Myocardial infarction |
Most common |
Collagen vascular disease |
Especially Lupus |
Trauma |
Surgical or accidental |
Metastatic disease |
Serosanguinous effusion |
Tuberculosis |
Uncommon except in AIDS |
Viral infection |
Coxsackie A and B virus |
Uremia |
18% in acute uremia |
- Other causes
- Serous fluid or transudate
- Congestive heart failure
- Hypoalbuminemia
- Irradiation
- Blood (hemopericardium)
- Rupture of ascending aorta or pulmonary trunk
- Coagulopathy
- Fibrin (produces exudate)
- Pyogenic infection, e.g. staph
- Uremia
- More common in chronic renal disease than acute
Imaging findings
- Conventional radiography
- Suggestive but not usually diagnostic
- "Water bottle configuration" is symmetrically enlarged cardiac silhouette
- Major DDX is cardiomegaly
- Loss of retrosternal clear space
- Non-specific and frequently not valid
- "Fat-pad sign"
- Produced by separation of retrosternal from epicardial fat line >2 mm
- Rapidly enlarging cardiac silhouette with normal pulmonary vascularity
- Echocardiogram
- Study of choice
- Echo-free fluid between the visceral and parietal pericardium
- Early effusions accumulate posteriorly first
- > 1cm is usually defined as a “large” effusion
- CT
- May detect small effusions (50cc)
- Fluid-filled space surrounding the myocardium
- Early effusions accumulate posteriorly first
Treatment
- Medical treatment depends on cause and may include
- Non-steroidal anti-inflammatory agents
- Colchicine
- Steroids
- Antibiotics
- Chemotherapeutic agents
- Pericardiocentesis
- Pericardial sclerosis for recurring effusions
- Tetracycline, doxycycline, 5-fluorouracil
- Pericardial window
- Video-assisted thoracic surgery (VATS)
- Allows for wide resection of pericardium
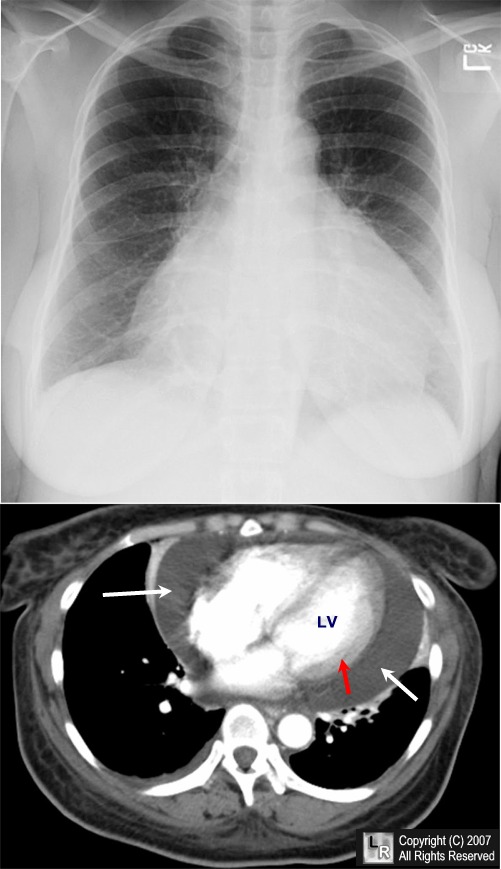
Pericardial effusion. Frontal chest radiograph (above) demonstrates a markedly enlarged cardiac silhouette. The differential diagnosis would include cardiomyopathy and pericardial effusion. A single axial, contrast-enhanced CT scan of the chest at the level of the heart shows a large pericardial effusion (white arrows) surrounding the contrast-filled heart (LV=left ventricle). The red arrow points to the myocardium.
For additional information about this disease, click on this icon if seen above.
For this same photo without the arrows, click here
|
|
|