|
|
Subcapsular Hematoma and
Renal Laceration
General considerations
- Incidence
- Renal trauma is most common of all GU trauma occurring in about 10% of patients with significant blunt or penetrating abdominal trauma
- Cause
- Motor vehicle accident
- Contact sports
- Falls and fights
- Less often penetrating wounds
- Mechanism
- Direct blow (>80%) frequently compressed and often lacerated by lower ribs
- Acceleration-deceleration injuries can produce renal artery tears
- Associated with other organ injury in 20% of cases
Clinical findings
- More than 95% have hematuria
- About 25% of patients with gross hematuria have significant injuries
- But, 24% of patients with renal pedicle injury have no hematuria
- Only 1-2% with microhematuria have a severe renal injury
Types of injuries
CT Classification of Renal Trauma |
CT Grade |
Injury |
Usual Treatment |
Grade I |
Superficial cortical laceration, contusion and/or perirenal hematoma |
Observation |
Grade II |
Deep corticomedullary laceration involving the collecting system |
Observation or surgery |
Grade III |
Renal crush injury and/or main vascular pedicle injury |
Surgery |
Grade IV |
Injury of the renal pelvis or the ureteropelvic junction |
Surgery |
- Renal contusion
- Superficial cortical laceration (75-85%)
- Small cortical laceration without calyceal disruption
- Complete cortical laceration
- Fracture communicating with calyceal system (10%)
- Extraluminal contrast material
- Separation of renal poles or fracture
- Crush injury
- Usually involves injury to the renal vascular pedicle (5%)
- Multiple separate renal fragments
- Lack of enhancement of part or all of kidney
- Extraluminal contrast material
- Subcapsular hematoma
Imaging Findings
- Contrast-enhanced CT of the abdomen and pelvis is the study of choice
- Delayed scans may be needed to detect extraluminal contrast
- Contusion
- Focal patchy areas of decreased enhancement
- Renal laceration
- Irregular linear hypodense parenchymal areas
- They may be hyperdense if they contain blood
- Fracture
- Laceration connecting two cortical surfaces
- Shattered kidney
- Multiple separated renal fragments with or without perfusion
- Subcapsular hematoma
- Superficial crescentic, usually hyperdense zone beneath renal capsule and compressing adjacent parenchyma
- Less common than perinephric hematoma
- Perinephric hematomas presents as a poorly-defined, hyper-attenuating collection between Gerota’s fascia and the renal parenchyma
- They do not usually deform the shape of the renal parenchyma, even when large
- Subcapsular or perinephric hematoma is usually proportional to extent of injury
- Rarely, a subcapsular hematoma may compress the kidney sufficiently to produce renal perfusion and result in hypertension –the Page kidney
- Segmental arterial injury (infarction)
- Wedge-shaped perfusion defect, which persists even with delayed imaging
- Usually treated conservatively as they either resolve spontaneously or heal with small scar
- Devascularized kidney
- Diffuse non-perfusion of kidney
- Most often from a clot that forms in an incompletely torn renal artery
- Renal vein thrombosis
- Persistent nephrogram on delayed scans
- Active extravasation of contrast from renal artery
- Attenuation as bright as nearby arteries
Injury |
How do you recognize it |
Contusion (75-80%) |
Focal patchy areas of decreased enhancement |
Laceration |
Irregular linear hypodense parenchymal areas |
Fracture |
Laceration connecting two cortical surfaces |
Crush injury |
Multiple separated renal fragments ± perfusion |
Calyceal or pelvic injury |
Extraluminal contrast |
Vascular pedicle injury |
Wedge-shaped or diffuse non-perfusion of kidney |
Subcapsular hematoma |
Superficial crescentic hypodense area compressing adjacent parenchyma |
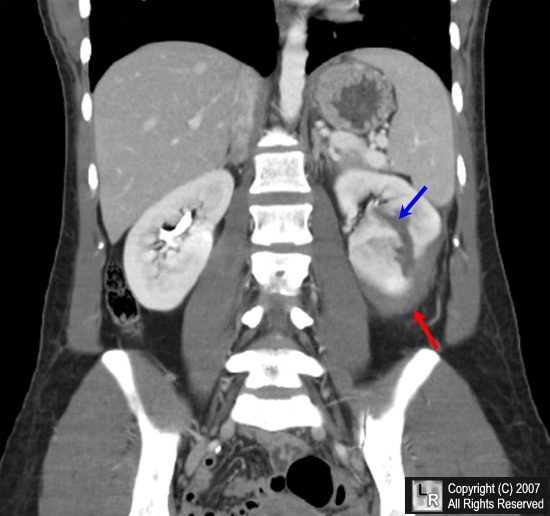
Subcapsular hematoma and laceration of left kidney. This is a coronal reconstruction of a contrast-enhanced CT scan of the abdomen and pelvis. There is a subcapsular fluid collection that compresses the adjacent renal parenchyma (red arrow). In addition, there is a lucency traversing the lower pole of the kidney that represents a renal laceration.
For additional information about this disease, click on this icon if above.
For this same photo without the arrows, click here
eMedicine Smith, J; Schauberger, J; Kenny, P; Cheer, A; and Lobera, A
|
|
|