|
|
Cardiogenic and Non-cardiogenic
Pulmonary Edema
General Considerations
- Increase in the fluid in the lung
- Generally, divided into cardiogenic and non-cardiogenic categories.
- Congestive heart failure is the leading diagnosis in hospitalized patients older than 65
Pathophysiology
- Fluid first accumulates in and around the capillaries in the interlobular septa (typically at a wedge pressure of about 15 mm Hg)
- Further accumulation occurs in the interstitial tissues of the lungs
- Finally, with increasing fluid, the alveoli fill with edema fluid (typically wedge pressure is 25 mm Hg or more)
Causes
- Cardiogenic pulmonary edema.
- Heart failure
- Coronary artery disease with left ventricular failure.
- Cardiac arrhythmias
- Fluid overload -- for example, kidney failure.
- Cardiomyopathy
- Obstructing valvular lesions -- for example, mitral stenosis

- Myocarditis and infectious endocarditis
- Non-cardiogenic pulmonary edema -- due to changes in capillary permeability
- Smoke inhalation.
- Head trauma
- Overwhelming sepsis.
- Hypovolemia shock
- Re-expansion

- By drainage of a large pleural effusion with thoracentesis
- Of the lung collapsed by a large pneumothorax
- High altitude pulmonary edema
- Disseminated intravascular coagulopathy (DIC)
- Near-drowning
- Overwhelming aspiration

- Heroin overdose
- Adult (acute) respiratory distress (deficiency) syndrome (ARDS)

- Clinical syndrome consisting of
- Pulmonary edema associated with severe respiratory distress
- Cyanosis refractory to oxygen administration
- Decreased lung compliance
- Lower pulmonary capillary wedge pressure (PCW < 18mm Hg) than cardiogenic pulmonary edema
- Most patients who survive have normal-appearing lungs
- Some patients develop pulmonary fibrosis
Clinical Findings
- Shortness of breath
- Hemoptysis
- Orthopnea
- Dyspnea on exertion
- Cough, wheezing
- Anxiety and restlessness
- Cyanosis
Imaging Findings
- Radiographic findings can lag behind physiologic changes
- The key findings of cardiogenic pulmonary edema
- Kerley B lines (septal lines)
- Seen at the lung bases, usually no more than 1 mm thick and 1 cm long, perpendicular to the pleural surface
- Pleural effusions
- Usually bilateral, frequently the right side being larger than the left
- If unilateral, more often on the right
- Fluid in the fissures
- Thickening of the major or minor fissure
- Peribronchial cuffing
- Visualization of small doughnut-shaped rings representing fluid in thickened bronchial walls
- Collectively, the above four findings comprise pulmonary interstitial edema
- The heart may or may not be enlarged
- When the fluid enters the alveoli themselves, the airspace disease is typically diffuse, and there are no air bronchograms
- Non-cardiogenic pulmonary edema
- Bilateral, peripheral air space disease with air bronchograms or central bat-wing pattern
- Kerley B lines and pleural effusions are uncommon
- Typically occurs 48 hours or more after the initial insult
- Stabilizes at around five days and may take weeks to completely clear
- On CT
- Gravity-dependent consolidation or ground glass opacification
- Air bronchograms are common

Non-Cardiogenic Pulmonary Edema. There is extensive, bilateral airspaces disease
centrally ;located in a bat-wing configuration with no evidence of pleural effusion,
fluid in the fissures or cardiomegaly.
Differential Diagnosis
Treatment
- Cardiogenic pulmonary edema and non-cardiogenic pulmonary edema, with the exception of ARDS, can resolve within hours to several days
- Cardiogenic pulmonary edema is usually treated with a combination of
- Diuretics
- Nitrates
- Natriuretic peptides
- Morphine
- Inotropic agents
- Dopamine, dobutamine, digoxin, etc.
- Angiotensin converting enzyme (ACE) inhibitors
- Beta-blockers
- For non-cardiogenic pulmonary edema, the predisposing condition should be treated
- Treatment is supportive
- Ventilator management.
- Antibiotic therapy, when necessary
- Corticosteroids
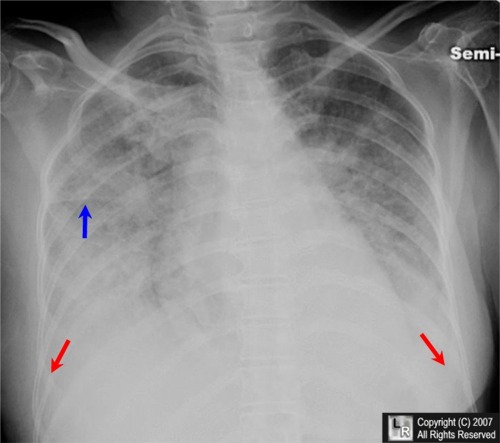
Pulmonary Alveolar Edema. There is extensive, bilateral airspaces disease with fluid in the
minor fissure (blue arrow) and bilateral pleural effusions (ref arrows). Although the heart is not
enlarged, the cause was still on a cardiogenic basis.
For additional information about this disease, click on this icon above.
For this same photo without the arrows, click here

Pulmonary Alveolar Edema, CT Scan. There is bilateral, almost-symmetrical perihilar airspace disease (with air bronchograms). There are multiple thickened septal lines seen in the periphery of the lungs. There are bilateral pleural effusions, larger on the right than the left.

Kerley B Lines, Congestive Heart Failure. Multiple, thin, short, white lines which are perpendicular to the chest wall at the lung base are seen (white oval) representing fluid which has leaked into the interlobular septae as a result of congestive heart failure, one of the signs of CHF.
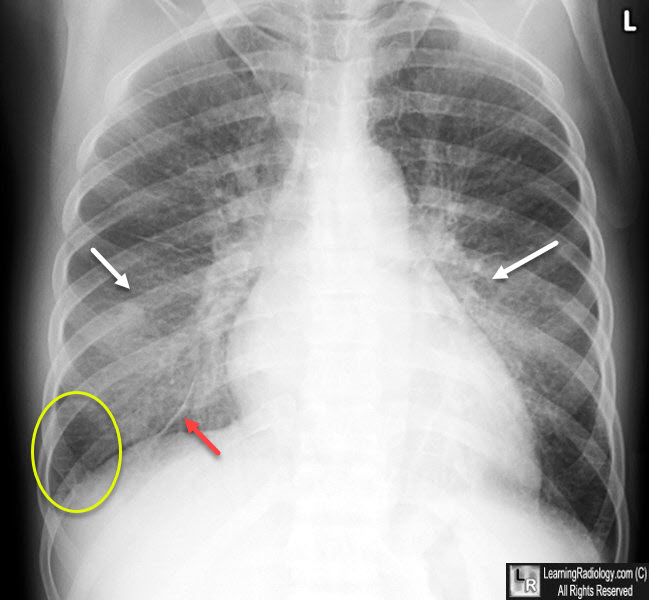
Congestive Heart Failure. There is bilateral, central airspace disease (white arrows), fluid in the inferior accessory fissure (red arrow) and Kerley B lines (yellow oval), all signs of congestive heart failure.
|
|
|