|
|
Hemothorax
General Considerations
- Hemothorax is blood in the pleural cavity
- Most often results from trauma to intrathoracic structures
- Exact distinction between a “bloody pleural effusion” and a hemothorax is not well defined
- Some use a fluid hematocrit >50% to define hemothorax
- Delayed appearance of a hemothorax can occur from rupture of a chest-wall hematoma or delayed perforation of an intercostal artery by a rib fracture
- Etiologies
- Blunt and penetrating trauma
- Penetrating trauma usually lacerates a blood vessel
- Primary or metastatic malignancy
- Anticoagulation
- Pulmonary embolism with infarction
- Tuberculosis
- Pulmonary arteriovenous fistulae
- Hereditary hemorrhagic telangiectasia
- Hemorrhage from another intrathoracic organ
- Thoracic aortic aneurysm
- Aneurysm of the internal mammary artery
- Intralobar and extralobar sequestration
- Abdominal pathology
- Pancreatic pseudocyst
- Splenic artery aneurysm
- Hemoperitoneum
- Catamenial
- Rare; related to thoracic endometriosis and episodic hemorrhage into the thorax that coincides with the patient's menstrual cycle
- Following lung or cardiac surgery
- Physiologic effects of a hemothorax
- The hemithorax can hold up to 4 L of blood, enough for an exsanguinating hemorrhage
- Clotting of blood may occur very quickly
- Upon lysis of the clots, the protein level in the pleural fluid rises, pulling transudative fluid into the pleural cavity
- This can result in an even larger pleural effusion
- Empyema can develop if the blood becomes infected
- Fibrothorax develops from fibrinous adhesions that lead to entrapment of the underlying lung
Clinical Findings
- Pain related to the chest wall injury
- Shock
- Tachypnea
- Dyspnea
- Hypoxemia
Associated Findings
Imaging Findings
- Upright conventional radiograph is usually the study of first choice
- About 350cc is needed to blunt the costophrenic sulcus on the frontal view
- Haziness of affected thorax will occur if the supine and a sufficient amount of blood is present
- CT is almost always performed in chest trauma
- Capable of detecting very small amounts of fluid and small pneumothoraces
Treatment
- One or two chest tubes are usually inserted, especially if the hemothorax is larger than 400cc
- Ideally, chest tube should be low and posterior fro fluid and high and anterior for air
- Surgery is usually indicated if
- One liter or more is evacuated immediately by chest tube
- Persistent bleeding, defined as 150-200cc/hour for 2-4 hours
- Recurrent transfusions are needed to maintain hemodynamic stability
- There is retained clot of 500cc or more
- Intrapleural instillation of fibrinolytic agents may also be used
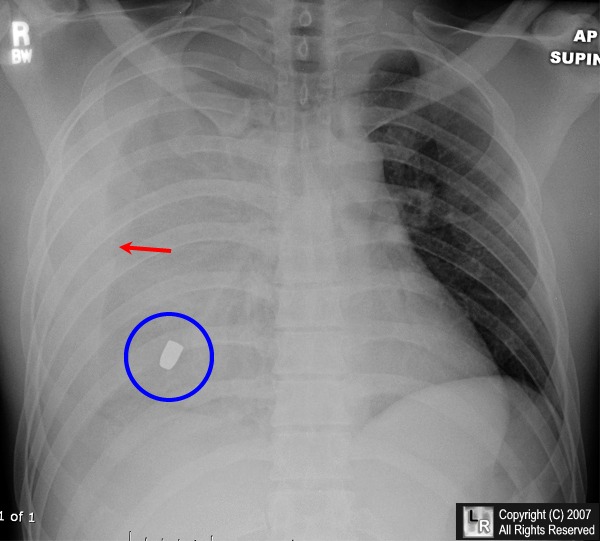
Hemothorax. There is complete opacification of the right hemithorax with slight shift of the trachea towards the left.
Fluid is seen tracking up the lateral margin of the thorax (red arrow). The clue to the diagnosis is the bullet (blue circle) which, on CT, was seen to lie within the pleural space.
For additional information about this disease, click on this icon above.
For this same photo without the arrows, click here
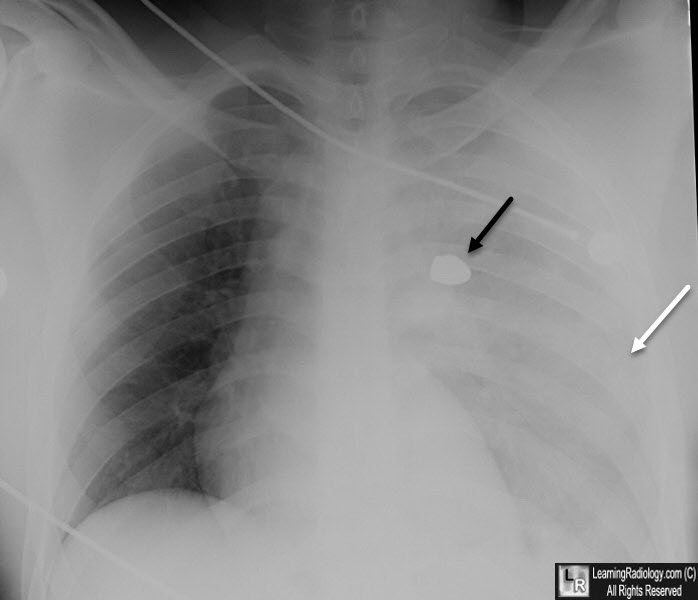
Hemothorax. There is complete opacification of the left hemithorax (white arrow) with slight shift of the heart towards the right.
The clue to the diagnosis again is the bullet (black arrow) which, on CT, was seen to lie within the pleural space.
eMedicine Mary C Mancini, MD and Jane M Eggerstedt, M
|
|
|