|
|
Uterine Rupture
General
- Most common in patients with previous cesarean delivery scars
- Rupture in the absence of a previous scar is uncommon
- Uterine trauma may occur following very prolonged or vigorous labor
- Especially if patient has relative or absolute cephalopelvic disproportion, and
Uterus has been stimulated with oxytocin or prostaglandins
- Trauma may result secondary to attempts to remove a retained placenta manually or with instrumentation
- Location
- Corpus with rupture before onset of labor
- Lower uterine segment during labor
Risk factors
- Patients with prior classic hysterotomy have higher rate of uterine rupture in subsequent pregnancies
- Those who have had 2 or more hysterotomies
- Those who are treated with prostaglandin agents and have undergone a previous caesarian have highest risk
- Those who undergo induction of labor have small increased risk
Clinical findings
- Acute abdominal pain
- “Popping” sensation
- Palpation of fetal parts outside of the confines of the uterus
- Repetitive or prolonged fetal heart rate deceleration
- Vaginal bleeding ─ early post-partum hemorrhage
Diagnosis is clinical
- Ultrasound may be useful if immediately available
Treatment
- Presence of uterine rupture dictates laparotomy be performed
- Treatment consists of immediate cesarean delivery with probable hysterectomy.
- Repair of uterus may be possible in some cases
Prognosis
- 2-20% maternal mortality
- 10-25% fetal mortality
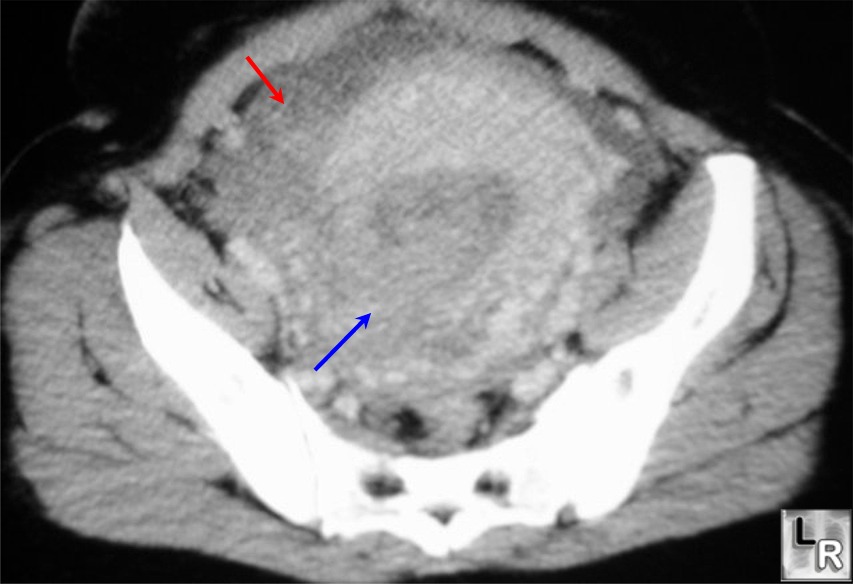
Uterine
rupture. Contrast-enhanced
CT
scan
through
the
pelvis
demonstrates
the
non-involuted
uterus
with a
large
discontinuity
representing
the
rupture
in the
right
posterolateral
wall
(blue
arrow).
There
is a
considerable
amount
of
blood
(red
arrow)
in the
pelvis.
The
pelvic
veins
are
dilated
from
the
recent
pregnancy.
|
|
|