|
Pulmonary Thromboembolic Disease
· Age
o Usually occurs
after 60 years of age
· Cause
o Most common
cause is deep vein thrombosis
(DVT) of lower extremity in
>90%
· Predisposing
factors
o Immobilization
(56%)
o Surgery (54%)
· Pathophysiology
o Clot from deep
veins of leg breaks off
o Travels via
venous system to right side of
heart
o Fragments in
right side of heart
o Showers lung
with emboli varying in size
§ On average > 6-8
vessels are embolized
· Clinical
findings
o Hemoptysis
(25-34%)
o Pleural friction
rub
o Thrombophlebitis
§ But only about
10-33% of patients with fatal
pulmonary embolism (PE) are
symptomatic for DVT
o Acute dyspnea
(81-86%)
o Pleuritic chest
pain (58-72%)
o Apprehension
(59%)
o Cough (54-70%)
o Tachycardia
o Tachypnea
o Accentuated 2nd
heart sound
o EKG changes
(83%)
§ Mostly
nonspecific
o Elevated levels
of fibrinopeptide-a (fpa)
= small peptide split off of
fibrinogen during fibrin
generation
o Positive d-dimer
assay (generated during clot
lysis)
· Location of
pulmonary emboli
o Bilateral emboli
in 45%
o Right lung only
in 36%
o Left lung only
in 18%
o Multiple emboli
[3-6 on average] in 2/3
· Distribution
by lobe
o Lower lobes more
often than upper lobes
o RUL (16%)
o RML (9%)
o RLL (25%)
o LUL (14%)
o LLL (26%)
· Site ─
central versus peripheral
o Central =
segmental or larger veins in
58%
o Peripheral =
subsegmental or smaller veins
in 42%
o In subsegmental
branches exclusively in 30%
o Emboli are
occlusive in 40%
· Resolution of
pulmonary embolism
o Through
fibrinolysis and fragmentation
o By time interval
§ In 8% by 24
hours
§ 56% by 14 days
§ 77% by 7 months
o By completeness
§ Complete in 65%
§ Partial in 23%
§ No resolution in
12%
§ Resolution less
favorable with increasing age
and cardiac disease
· Embolism
without infarction (90%)
o Dual blood
supply of lungs ─ pulmonary
and bronchial
· Imaging
findings in embolic disease
without infarction
o Normal chest
film common
o Normal chest
x-ray has a negative
predictive value of only 74%
o Plate-like
(subsegmental, discoid)
atelectasis
o Lobar
consolidation in lower lung
zones and pleural effusion
(most common findings with the
lowest positive predictive
value)
o Westermark sign
represents an area of oligemia
(due to vasoconstriction
distal to embolus)
§ Uncommonly seen
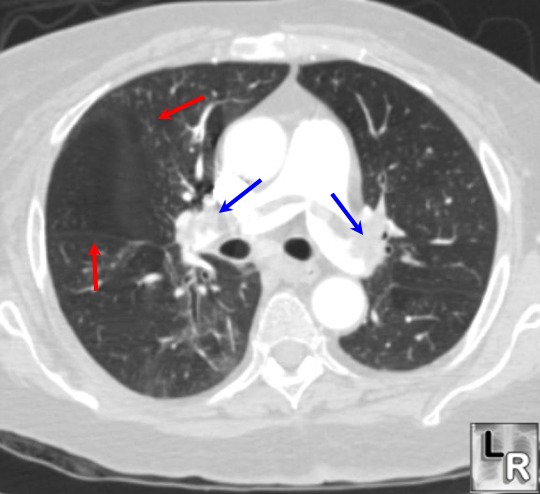
Axial CT image just below level
of tracheal bifurcation
demonstrates large
intraluminal filling defects
in both right and left
pulmonary arteries (blue arrows) representing a "saddle
embolus" straddling
the pulmonary arteries. An apparent area of oligemia is seen in the region of the fissure (red arrows)
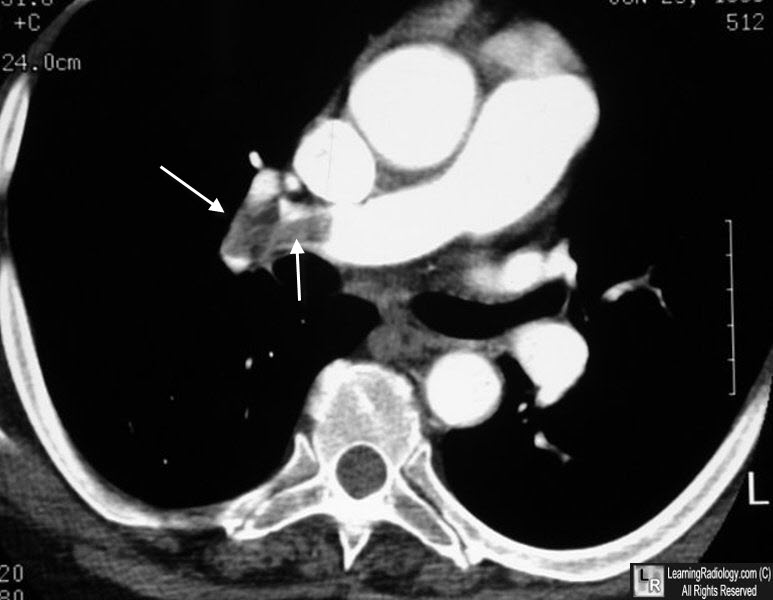
Pulmonary embolism. There is a large filling defect (white arrows) in the right pulmonary artery representing clot.
o Fleischner sign
refers to local widening of
artery by impaction of embolus
(due to distension by clot /
pulmonary hypertension
developing secondary to
peripheral embolization)
o "Knuckle sign"
is term used for abrupt
tapering of an occluded vessel
distally
· Imaging
findings in embolism with
infarction
o Segmentally distributed
wedge-shaped consolidation
(54%)
§ With or without
cavitation
o Hampton hump is
a pleural-based area of
consolidation in the form of a
truncated cone with base
against pleural surface
o Pleural effusion
in slightly over 50%
§ Thoracentesis
· Bloody (65%)
· Predominantly
PMNs (61%)
· Exudate (65%)
o Usually no
air-bronchogram because of
hemorrhage into alveoli
o "Melting sign"
is the sign that refers to
disappearance of the
opacification within few days
to weeks from periphery toward
center
o Fleischner lines
= long-line shadows (fibrotic
scar)
o Plate-like
(subsegmental, discoid)
atelectasis (27%)
o Cardiomegaly or
CHF (17%)
o Elevated
hemidiaphragm (17%)
o Subsequent
nodular or linear scar more
often than pneumonia leads to
scarring
· CT findings (can be equal to angio in
detection of emboli within
proximal arteries):
o Subsegmental
intraluminal filling defects
may not be detectable
o Detection is
poorer in middle lobe and
lingular branches
o Peripheral
wedge-shaped lung densities
with the triangle base
adjacent to pleural surface
o Peripheral
rimlike contrast enhancement
in a pulmonary artery
o Intraluminal
filling defect in pulmonary
artery
· NUC (VQ scan =
guide for angiographic
evaluation)
· Interpreted in
reference to Biello or PIOPED criteria
o Low- /
intermediate-probability scans (73%)
§ Additional
studies recommended
o High-probability
scan
§ In 12% normal
angiogram
· Angiographic
findings
o Intraluminal
defect (94%)
o Abrupt
termination of pulmonary
arterial branch
o Pruning and
attenuation of branches
o Wedge-shaped
parenchymal hypovascularity
o Absence of
draining vein in affected
segment
o Tortuous
arterial collaterals
o Complications of
pulmonary angiography
§ Arrhythmia,
endocardial injury, cardiac
perforation, cardiac arrest,
contrast reaction
|