|
|
Achalasia
Definition
- Form of esophageal dysmotility characterized by loss of distal
esophageal peristalsis and failure of lower esophageal sphincter relaxation
Etiology & Pathophysiology
- Usually idiopathic in origin
- Degeneration of neurons within the myenteric plexus of the
esophageal smooth muscle
- Neuronal destruction is typically inflammatory in nature
- Histologically: lymphocytic infiltrate surrounding the plexus
- Predominantly involves the nitric-oxide producing inhibitory neurons
- Cause smooth muscle relaxation by inhibiting the acetylcholine
producing excitatory neurons
- Loss of inhibitory input results in unopposed contractile stimulation and
aperistalsis
- Acetylcholine producing neurons (which stimulate smooth muscle
contraction) are relatively spared in this degenerative process
Types
- Primary achalasia (idiopathic)
- Unknown cause of inflammatory neuronal degeneration
- Secondary achalasia (pseudoachalasia)
- Recognized pathologic causes of esophageal motility disorders often indistinguishable from primary achalasia
- Malignancy (especially gastric cancer)
- MEN, Type 2B
- Chagas’ disease
- Juvenile Sjögren’s
- Amyloidosis
- Chronic idiopathic intestinal
- Sarcoidosis
- Pseudo-obstruction
- Neurofibromatosis
- Eosinophilic gastroenteritis
- Fabry’s disease
- Scleroderma
Epidemiology
- Annual incidence of 1 case per 100,000
- Men and women affected equally
- Occurs at any age
- Typically between 25-60 years of age
- Onset rare before adolescence
Clinical Findings
- Dysphagia for solids and liquids predominate (85-95% of patients)
- Dysphagia for liquids especially should prompt evaluation for achalasia
- Difficulty belching
- Hiccups
- Weight loss
- Chest pain
- Usually secondary to failure of LES relaxation
- More common in younger patients and tends to regress
- Regurgitation of retained material in esophagus, especially upon lying down
- May lead to recurrent aspiration
- Heartburn in 40-60%
- Tend to have lower LES pressures than those without GERD
- Increased incidence of esophageal cancer
- Usually squamous cell
- Surveillance endoscopy not recommended (usually seen 15-20 years after development of achalasia)
Imaging Findings
- Barium studies
- 95% diagnostic accuracy
- Early/Stage I
- Primary peristaltic waves absent with abnormal distal peristalsis
- Only minimal narrowing of the GE junction
- Occasionally may see nonpropulsive peristaltic waves in the esophageal body (“vigorous achalasia” secondary to tertiary waves)
- Progressive disease
- “Bird’s beak” appearance of GE junction
- Distal esophagus makes right angle before entering stomach
- Hurst phenomenon
- With the patient upright, barium builds up to a point where the
hydrostatic pressure of the barium overcomes the LES pressure
- Occasional “spurt” of barium through the GE junction as it is intermittently forced open
- Dilated, aperistaltic esophageal body; may assume a sigmoid shape
- Severe disease
- Significant esophageal body dilation with large amounts of fluid/food retention
- Entire esophagus atonic in late stages
- Chest x-ray
- With severe disease, may readily see the large, dilated esophagus
with air fluid level at the aortic arch or above
- Stomach bubble frequently absent
- CT Scan
- Not typically used for diagnosis
- Seen as dilated luminal structure with retained debris and narrowing
at level where it enters the stomach
- Manometry
- Usually required for confirmation of diagnosis
- Elevated resting LES pressure
- Incomplete LES relaxation
- Absence of peristalsis
- Endoscopy
- Must rule out malignancy
- Reveals dilated esophagus with normal mucosa
- Retained fluid/food
- Possible Candidal infection secondary to esophageal stasis
- Endoscope should pass easily through LES with gentle pressure applied
- Unlike strictures caused by neoplasms, fibrosis etc
Differential Diagnosis
- Reflux esophagitis with stricture
- Narrowing is usually higher than the EG junction
- Normal esophageal peristalsis
- Carcinoma
- Only minimal dilation with normal peristalsis
- Scleroderma
- Barium should empty when patient is upright
- Other associated GI abnormalities
- Chagas disease
- Not distinguishable by x-ray; history needed
Treatment
- Medical therapy
- Nitrates, calcium channel blockers (nifedipine)
- Cause smooth muscle relaxation but with limited success
- Pneumatic dilation of the LES
- Tears muscle fibers of LES, thus weakening it
- Varying protocols regarding type and diameter of dilator,
balloon inflation pressure and rate at which it is inflated, duration of
inflation, and
number of inflations per session
- Good short-term results, but many patients require further intervention,
with successive dilations adding little benefit
- Potential complications of esophageal perforation (2-6%) and GERD
- Surgical myotomy
- LES muscle fibers cut
- Laparoscopy becoming more popular
- Good relief of symptoms in majority of patients with complication rate
similar to that of dilation
- Superior method for achieving better long term results
- Debate as to whether fundoplication is necessary to prevent
longstanding GERD
- Botulinum toxin injection
- Inhibits release of excitatory acetylcholine from nerve endings
(thus causing lower LES pressures)
- Good short-term results, but long term efficacy unknown


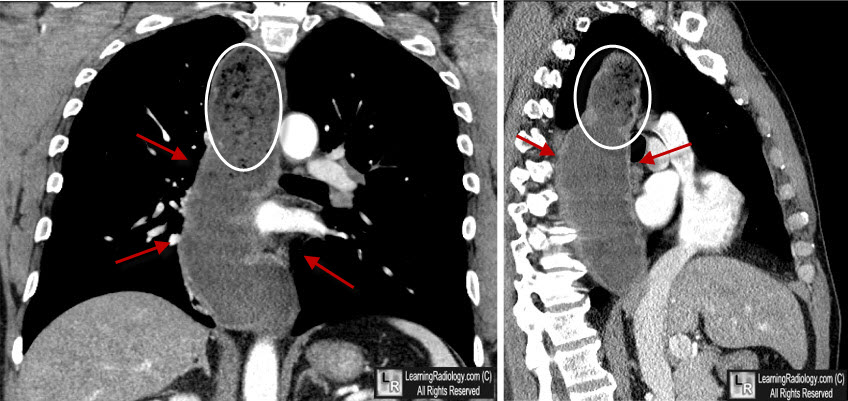
Achalasia. Upper: There is a large air-filled tubular structure that represents the dilated
esophagus (white arrows). Lower: An esophagram shows a massively dilated esophagus
(yellow arrows) down to the esophagogastric junction consistent with achalasia.
For these same photos without the arrows, click here and here
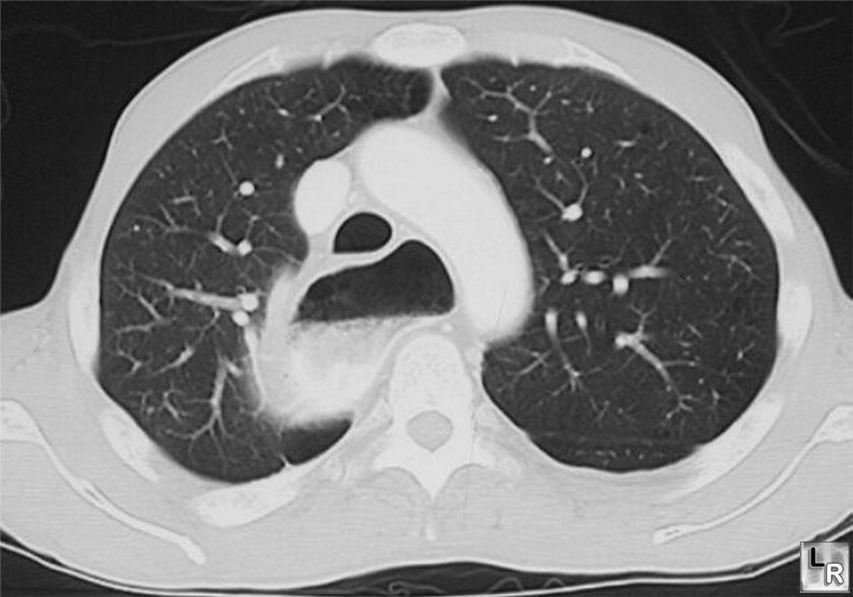
CT scan of the chest demonstrates a markedly dilated esophagus
containing barium, debris and a fluid level
For more information, click on the link if you see this icon 
|
|
|