|
|
Serous Ovarian Tumors
Submitted by Ron Gefen, MSIV
General
Most common of six types of epithelial tumors which derive from surface mesothelial cells of the ovary
70% are benign (serous cystadenoma)
10% have low malignant potential
20% are malignant (serous cystadenocarcinoma)
Transabdominal and/or transvaginal ultrasound is the most valuable diagnostic study in determining area of origin, size, and cystic versus solid make-up
Screening finds adnexal cysts in up to 15% of postmenopausal woman
Only 3% of ovarian cysts are malignant
Doppler color flow imaging can be helpful in differentiating malignant from benign masses
Malignancies are rich in neovascularization and therefore have lower resistive and pulsatile indices
Gray-scale ultrasound for diagnosis of ovarian malignancy is 62 – 100% sensitive and 77 – 95% specific
Treatment involves surgical removal for all serous tumors
Serous Cystadenoma
- 20% of all benign ovarian tumors
- Women usually between 20 - 60 years
- Present clinically as cystic adnexal masses
- Increasing abdominal girth
- 15% are bilateral
- Imaging findings
- Average 5-10cm (frequently grow larger)
- May be indistinguishable from simple cysts
- Or they may have thin septations and occasionally papillary projections
- Tend to be unilocular, but may also be multilocular
- Lined by a single layer of non-ciliated cuboidal to tall columnar epithelium
- Straw-colored fluid within them is usually blood tinged
Serous Cystadenocarcinoma
- Most common malignant tumor of the ovary
- Up to 50% are derived from malignant transformation of serous cystadenomas
- 30% bilateral at time of diagnosis
- Occur mostly from age 40 – 60 years
- Histological characterization
- Cells vary from well-differentiated to poorly differentiated tumors
- Ciliated cells common
- Psammoma bodies (calcified concretions) present in 33%
- Imaging findings
- Predominantly cystic but with variable solid component
- Usually multi-loculated
- Solid areas can have areas of necrosis and hemorrhage
- Many >10cm at time of diagnosis
- May produce ascites and omental caking if metastases
- Intra-abdominal dissemination at initial time of surgery common
- Staging for Primary Carcinoma of the Ovary
- Stage I. Growth limited to the ovaries
- Ia. One ovary involved
- Ib. Both ovaries involved
- Ic. Ia or Ib and ovarian surface tumor, ruptured capsule, malignant ascites, or malignant peritoneal cytology
- Stage II. Disease extension from the ovary to the pelvis
- IIa. Extension to the uterus or fallopian tube
- IIb. Extension to other pelvic tissues
- IIc. IIa or IIb and ovarian surface tumor, ruptured capsule, malignant ascites, or malignant peritoneal cytology
- Stage III. Disease extension to the abdominal cavity
- IIIa. Abdominal peritoneal surfaces with microscopic metastases
- IIIb. Tumor metastases <2 cm
- IIIc. Tumor metastases >2 cm, or metastatic disease in the pelvic, para-aortic or inguinal lymph nodes
- Stage IV. Distant metastatic disease
- Malignant pleural effusion
- Pulmonary parenchymal metastases
- Liver or splenic parenchymal metastases
- Metastases to the supraclavicular lymph nodes or skin
- Cancer staging dictates treatment and predicts prognosis
- Stage 1
- Usually TAH and BSO
- With or without chemotherapy
- > Stage 1
- Usually TAH and BSO
- Surgical debulking of tumor, if needed
- Chemotherapy
- 5-year survival rate for all types is 20 - 35%
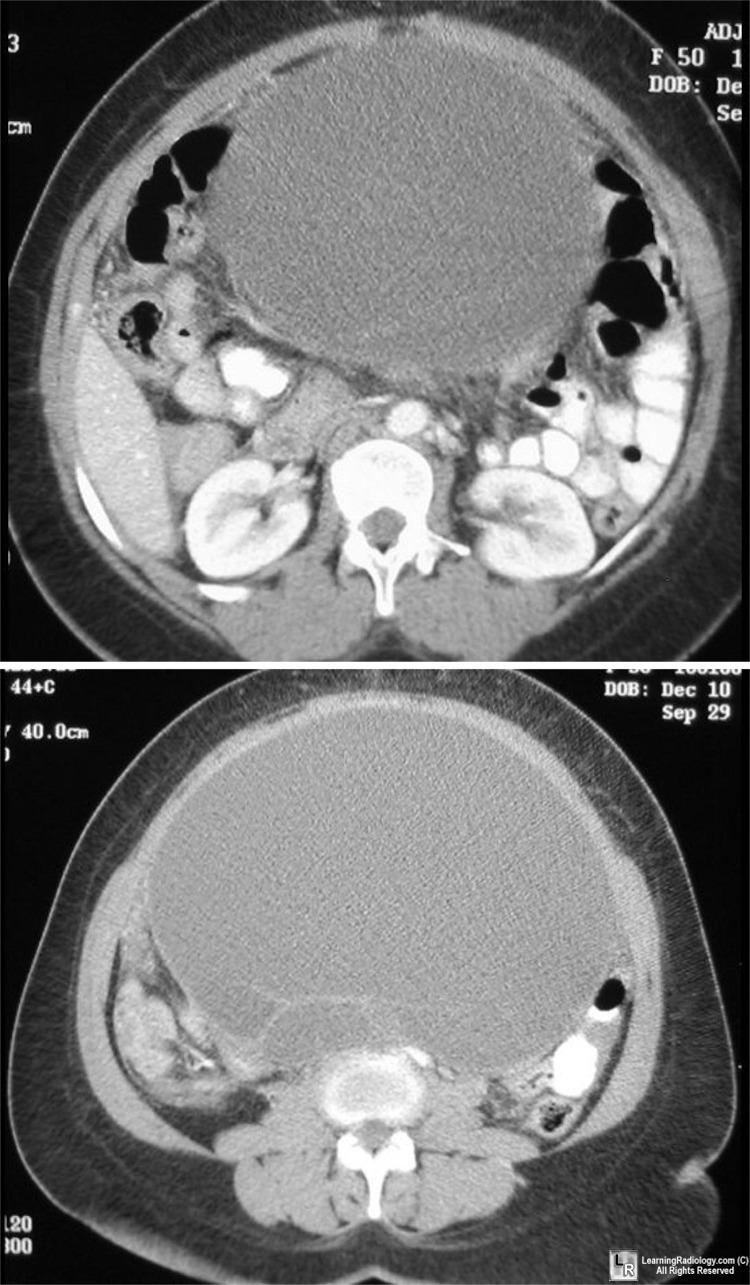
Serous ovarian tumor. CT of lower abdomen demonstrates a
large, fluid-filled and septated mass arising from the pelvis
|
|
|