|
|
Appendicitis
- Incidence
- 7-12% in Western world population
- Peak age
- Etiology
- Obstruction of appendiceal lumen by
- Lymphoid hyperplasia
- Fecolith
- Foreign bodies
- Stricture
- Tumor
- Parasite
- Crohn’s disease
- Clinical findings
- RLQ pain over appendix is a positive McBurney
sign
- Leukocytosis
- Fever
- Nausea and vomiting
- Relatively higher rate of misdiagnosis in
women between ages 20-40
- May have an atypical location
- Imaging Findings
- Abdominal plain film (abnormalities seen in
<50%)
- Plain-film findings become more distinctive
after perforation, while clinical findings subside
- May simulate other diseases
- Calcified, frequently laminated,
appendicolith in RLQ (in 7-15%)
- Appendicolith and abdominal pain = 90%
probability of acute appendicitis
- Appendicolith in acute appendicitis means
a high probability for perforation
- "Cecal ileus" = local paralysis
- Small bowel obstruction pattern
- Soft-tissue mass and paucity or absence of
intestinal gas in RLQ (more often with perforation)
- Extraluminal gas bubbles (again more often
in perforation)
- Large pneumoperitoneum is rare because
etiology of appendicitis involves obstruction of a very small
lumen
- Focal increase in thickness of lateral
abdominal wall
- Loss of properitoneal fat line on right side
- BE / UGI (accuracy 50-84%):
- Failure to fill appendix with barium (normal
finding in up to 35%)
- Indentation along medial wall of cecum (from
edema at base of appendix / matted omentum / periappendiceal abscess)
- US (77-94% sensitive, 90% specific, 78-96%
accurate)
- Useful in ovulating women (false-negative
appendectomy rate in males 15%, in females 35%):
- Visualization of noncompressible appendix as a blind-ending tubular aperistaltic structure (seen only in
2% of normal adults, but in 50% of normal children)
- Target appearance of >6
mm in total diameter on cross section (81%)
- Mural wall thickness >2 mm
- Diffuse hypoechogenicity (associated with higher frequency of
perforation)
- Lumen may be distended with anechoic / hyperechoic material
- Loss of wall layers
- Visualization of appendicolith (6%)
- Localized periappendiceal fluid collection
- Prominent hyperechoic mesoappendix / pericecal fat
- Color Doppler US:
- Increased conspicuity from increase (in size
+ number) of vessels in and around the appendix
- Decreased resistance of arterial waveforms
- Continuous / pulsatile venous flow
- CT (87-98% sensitive, 83-97% specific, 93%
accurate)
- Distended lumen
- Circumferentially thickened and enhancing
wall
- Appendicolith = homogeneous / ringlike
calcification (25%)
- Periappendicular inflammation-linear streaky densities in periappendicular fat
- Pericecal soft-tissue mass
- Abscess
- Poorly encapsulated
- Single or multiple fluid collection(s)
with air
- Extraluminal contrast material
- Focal cecal wall thickening (80%)
- "Arrowhead" sign = funnel of contrast medium
in cecum centering about occluded orifice of appendix
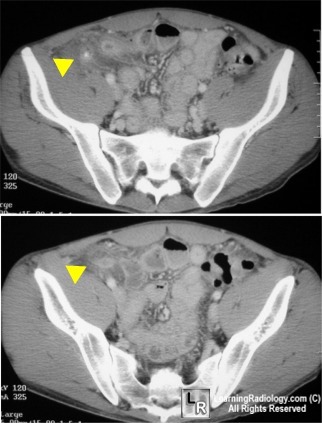
Yellow arrowheads point to appendicolith (upper) and
appendix
with thickened and enhancing wall and peri-appendiceal stranding (lower)
- Complications
- Differential diagnosis (DDx)
- Colitis
- Diverticulitis
- Epiploic appendagitis
- Infectious enteritis
- Intussusception
- Crohn’s disease
- Mesenteric lymphadenitis
- Ovarian torsion
- Pelvic inflammatory disease
- Treatment
- Appendectomy
- Finding of appendicolith is sufficient
evidence to perform prophylactic appendectomy in asymptomatic
patients (50% have perforation / abscess formation at surgery)
|
|
|