|
|
Giant Cell Tumor
- Probably arise from zone of osteoclastic
activity in skeletally immature patients
- Incidence
- ~ 4% of all primary bone tumors
- ~ 20% of benign skeletal tumors
- Histology
- Multinucleated osteoclastic giant cells
intermixed throughout a spindle cell stroma
- Age
- > 98% after epiphyseal plate fusion
- Most between 20 and 40 years
- M:F = 1:1
- Clinical
- Tenderness
- Pain at affected site
- Weakness
- Sensory deficits (if in spine)
- Location:
- 85% in long bones
- Lower extremity (50-60% about knee)
- Distal femur > proximal tibia
- Upper extremity (away from elbow):
- Distal radius > proximal humerus
- 15% in flat bones
- Pelvis
- Sacrum near SI joints
- Skull
- Site in bone
- Eccentric
- Metaphyseal
- Adjacent to epiphyseal line
- Subarticular if epiphyseal plate is fused
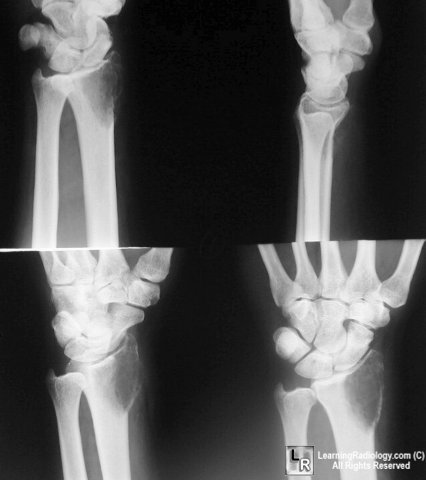
Four views of the wrist show a lytic,
eccentric and slightly expansile, geographic
lesion in the distal radius and extends to the end of the bone
- Appearance
- Expansile
- Solitary lytic bone lesion
- May be quite large at diagnosis
- No reactive sclerosis
- No periosteal reaction in absence of fracture
- May break through cortex with cortical
thinning
- Soft-tissue invasion (25%)
- Pathologic fracture (5%)
- Destruction of vertebral body with secondary
invasion of posterior elements (DDx: ABC, osteoblastoma)
- Frequently demonstrate vertebral collapse
- Can involve adjacent vertebrae and disk
(like discitis) and can cross sacroiliac joint
- May cross joint space in long bones
(exceedingly rare)
- Nuclear medicine findings
- Diffusely increased uptake
- May have "doughnut" sign of central photopenia
- Angiographic findings
- CT findings
- Tumor has soft-tissue attenuation
- May contain foci of low attenuation
(hemorrhage/necrosis)
- Well-defined margins
- May have thin rim of sclerosis
- MR findings
- Heterogeneous signal intensity with low to
intermediate intensity on T1WI + T2WI (63-96%) due to collagen +
hemosiderin content
- Focal cystic areas
- Low-signal-intensity pseudocapsule
- Complications and associations
- 15% malignant within first 5 years
- Much more often in males (M:F = 3:1)
- Metastases to lung
- May be associated with
- Paget disease (in 50-60% located in skull +
facial bones)
- Prognosis
- Locally aggressive
- 40-60% recurrence rate
- Treatment
- Complete resection + radiation therapy
- DDx:
- Aneurysmal bone cyst
- Brown tumor (lab values)
- Cartilaginous tumor
- Chondroblastoma (open epiphyses)
- Enchondroma (not epiphyseal)
- Chondromyxoid fibroma (rare)
- Chondrosarcoma
- Fibrous dysplasia
|
|
|