|
|
Abdominal Aortic Aneurysm
General Considerations
- Focal
widening >3 cm
- Normal size of abdominal aorta >50
years of age:
Prevalence:
- Increases with age
- Greater with atherosclerotic disease
- Male predominance
- Whites: Blacks = 3:1
- Risk factors:
- male
- age >75 years
- white race
- prior vascular disease
- hypertension
- cigarette smoking
- family history
- hypercholesterolemia
Associated with:
- visceral +
renal artery aneurysm (2%)
- isolated iliac
+ femoral artery aneurysm (16%)
- common iliac
(89%), internal iliac (10%), external iliac (1%)
- stenosis /
occlusion of celiac trunk / SMA (22%)
- stenosis of
renal artery (22-30%)
- occlusion of
inferior mesenteric artery (80%)
- occlusion of
lumbar arteries (78%)
- Growth rate of aneurysm of 3-6 cm in
diameter:
Clinical
- asymptomatic (30%)
- abdominal mass
(26%)
- abdominal pain
(37%)
- Location
- infrarenal (91-95%) with extension into iliac arteries (66-70%)
Imaging findings
- Plain film
- mural calcification (75-86%)
- US:>98% accuracy in size measurement
- CT-non-contrast enhanced
- perianeurysmal fibrosis (10%), may cause ureteral obstruction
- "crescent sign" = peripheral
high-attenuating crescent in aneurysm wall (= acute intramural
hematoma) = sign of impending rupture
- CT-contrast-enhanced
- ruptured aneurysm
- anterior displacement of kidney
- extravasation of contrast
material
- fluid collection / hematoma
within posterior pararenal + perirenal spaces (see below)

Abdominal Aortic Aneurysm. There is a large contrast-containing abdominal aortic aneurysm just anterior to the spine with evidence of extraluminal extravasation of contrast along the left paravertebral gutter.
- free intraperitoneal fluid
- contained leak
- laminated mural calcification
- periaortic mass of mixed /
soft-tissue density
- lateral "draping" of aneurysm
around vertebral body
- Angio
- focally widened aortic lumen >3 cm
- apparent normal
size of lumen secondary to mural thrombus (11%)
- mural clot
(80%)
- slow antegrade flow of contrast
medium
- Contained rupture = extraluminal
hematoma / cavity
- absent parenchymal stain = avascular
halo
- displacement + stretching of aortic
branches
- Complications:
- Rupture (25%)
- into retroperitoneum: commonly on
left
- into GI tract: massive GI
hemorrhage
- into IVC: rapid cardiac
decompensation
- Incidence: aneurysm <4 cm in
10%, 4-5 cm in 23%, 5-7 cm in 25%, 7-10 cm in 46%, >10 cm in 60%
- Symptoms of rupture
- sudden severe abdominal pain ±
radiating into back
- faintness, syncope,
hypotension
- Prognosis:64-94% die before
reaching hospital
- Increased risk: size >6 cm,
growth >5 mm / 6 months, pain + tenderness
- Peripheral embolization
- Infection
- Spontaneous occlusion of aorta
- Prognosis:17% 5-year survival without
surgery
- 50-60% 5-year survival with surgery
- Treatment
- surgery recommended if >5 cm in
diameter;
- 4-5% surgical mortality for
nonruptured
- 30-80% for ruptured aneurysm
- Postoperative Complications
- Left colonic ischemia (1.6%) with
10% mortality
- Renal failure (14%)
- 0-8% mortality rate for elective
surgery
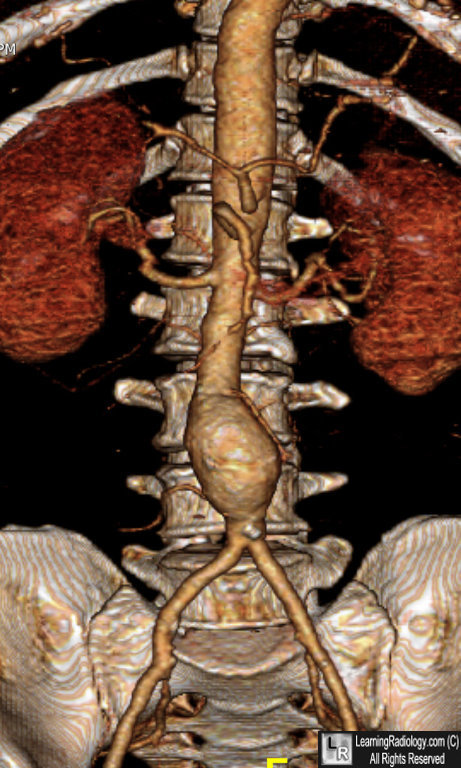
Abdominal Aortic Aneurysm. Three-dimensional CT reconstruction show a saccular dilatation of the abdominal aorta just distal to the renal arteries, not extending into the femoral arteries.
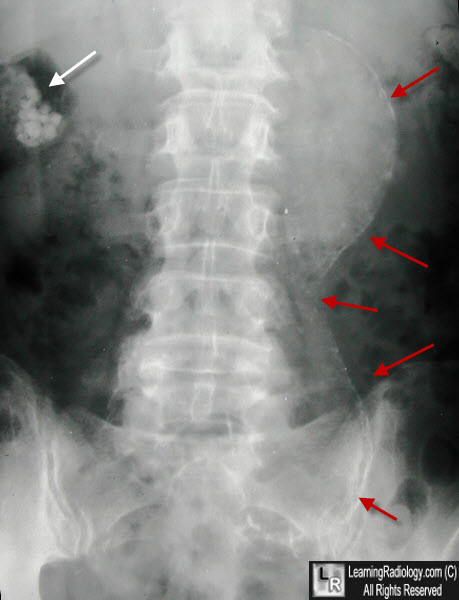
Abdominal Aortic Aneurysm. There is calcification in the left lateral wall of a huge, bi-lobed abdominal aortic aneurysm (red arrows). Incidental note is made of gallstones in the right upper quadrant (white arrow).
|
|
|